Increasing life expectancy and chronic disease prevalence have resulted in a rise in demand for specialist services.1 In Australia, referrals from general practitioners (GPs) to non-GP specialists (hereafter denoted as ‘specialists’) rose 23% between 2004/05 and 2013/14.2,3 This growth, and the associated delay in obtaining specialist input, can lead to a deterioration in health, increasing the likelihood of avoidable hospital attendance.4 In addition, systems for GPs to access specialist support for patients are limited to in-person specialist care referrals5 or informal methods, such as telephoning personal specialist contacts for advice.6 Internationally, eConsultant models have been trialled to address demands on healthcare systems without requiring face-to-face specialist input.7–9 They provide a formalised, efficient and documented method for family physicians to access specialist support in a way that is timely, convenient to both provider and patient, resource efficient and of educational value.
eConsultant episodes are defined as asynchronous GP-to-specialist communications over a secure electronic medium that involves sharing patient-specific information for the purpose of decision support or guidance regarding patient care.10 Synchronous videoconferencing platforms require simultaneous availability of the GP and specialist, and typically also the patient,8,10 whereas GP access to an asynchronous provider-to-provider eConsultant can be more feasible, allowing busy clinicians to connect during clinical downtime.7,10 Significantly reduced wait times for specialist input and substantial avoidance of face-to-face hospital visits are established outcomes of the eConsultant approach internationally.7,8,10,11 While the cost savings7 and improved patient health outcomes12 of the eConsultant model are less extensively researched, findings are promising. In addition, facilitating GP access to specialist support through better integrated primary–secondary care is associated with improved communication, access and patient-centeredness.13–15
Flexible in its application and feasible in a variety of settings, the eConsultant model has the capacity to both address the ‘supply–demand mismatch’16 for specialty care in populations with access disadvantage, and intervene early in the disease process, reducing avoidable hospital utilisation. Complex or chronic disease management is within the purview of the adult general physician specialty and is well suited to the eConsultant model.17,18 Generally well accepted by both primary care and specialist providers, the eConsultant model of care facilitates decision support for GPs, an element of care of particular importance in the management of patients with complex or chronic disease.7
Asynchronous electronic GP-to-specialist consultation services have been researched and successfully implemented in the USA, Canada and Europe.7,8,19 However, applications in the Australian setting are limited, with the exception of a ‘store and forward’ teledermatology initiative with specialist input using clinical photos from doctors in rural and remote communities.20 The aim of this pilot study was to assess the feasibility, acceptability and implementation of an asynchronous GP-to-general-physician eConsultant outpatient substitution program in the Australian healthcare setting.
Methods
Study design
The pilot study was conducted in five Queensland general practices, commencing with proof of concept in an urban practice in February 2018 and extending to four rural/remote practices (one private, one Aboriginal Community Controlled Health Organisation and two Royal Flying Doctor Service general practices) from November 2019. All practices are ongoing in the program. Evaluation included a retrospective review of clinical and patient data and a two-question open-ended eQuestionnaire for key stakeholders (providers and patients). Ethical approval was obtained from the University of Queensland Human Research Ethics Committee (approval number: 2018000253).
The eConsultant model
The study model of care is based on the Canadian prototype (Figure 1).21
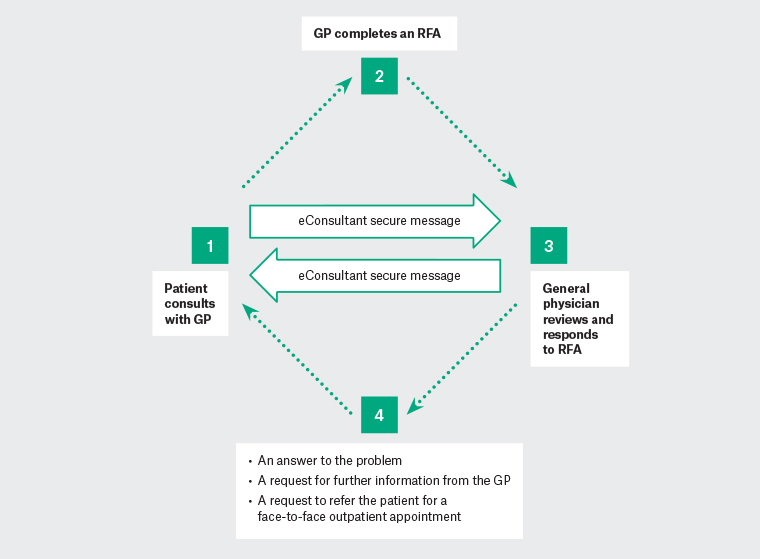
Figure 1. The eConsultant model of care
GP, general practitioner; RFA, request for advice
The aim is to provide support from a general physician, within three business days (72 hours), for GPs and patients who would otherwise require an outpatient department (OPD) referral. GPs send a request for advice (RFA) template to a remote physician (the eConsultant) employed by the Mater Hospital, Brisbane (Mater). The RFA is sent via a secure messaging platform (Medical Objects) and includes a clinical summary and a specific question/s about the next steps in care. Fields are automatically populated from the GP’s clinical information system (Medical Director, Best Practice, Stat). The eConsultant has three response options: an answer to the problem, a request for further information or a request to refer the patient for a face-to-face OPD appointment. Following patient consent and dispatch of the RFA, GPs advise patients to schedule a timely follow-up appointment to discuss the eConsultant advice. All treatment decisions are made in partnership with the patient and on the understanding that the clinical scenario is substitutable with a usual care specialist referral. On receipt of the RFA, the Mater allocates patients a unique record number and medical record, which may be a new or an existing one if they are known to the health service, where a copy of the RFA and physician’s response are stored. This ensures efficient articulation of the new approach with existing processes. GPs use the same billing practice as they would for an OPD referral, and the eConsultant is funded by the Queensland eConsultant Partnership Program (QePP) at the specialist’s current face-to-face session rate. The eConsultant was recruited through the Director of Internal and Perioperative Medicine who consented to participate in the study. Subsequently, two other general physicians expressed interest and have been recruited to the program.
Practices
The urban proof-of-concept practice was recruited through the research team’s general practice networks. The rural/remote practices were approached and recruited in collaboration with the Western Queensland Primary Health Network (WQPHN). There were seven GPs at the urban practice; one rural/remote practice consisted of a sole practitioner, and there were two GPs at each of the other practices. Secure email was initially used in the urban practice; however, this was modified to secure messaging, which enabled interoperability and safe, seamless and secure information sharing between providers without practice email encryption costs. GPs and administration staff received 30 minutes’ online training in sending and using an RFA.
Participants
Eligible patients were consenting adults (aged ≥18 years) who would otherwise require a specialist OPD referral (Queensland Health OPD Referral Category 1–3).22 Participants were recruited by the GP if it was determined that an RFA to the eConsultant would meet their clinical needs.
Data measures and collection
Patient demographics (sex, date of birth), clinical data (comorbidities, primary clinical problem for the RFA) and referring GP name and practice were in the main automatically populated to the RFA from the general practice software as would occur for OPD referrals. The only data collected directly by the eConsultant were the RFA question/s. The eConsultant also recorded the question type (ie diagnosis, management or monitoring), number of requests for more information, the RFA response (eg an answer to the problem; a request the patient be referred for a face-to-face OPD appointment) and time (minutes) spent preparing the response. GPs provided the time (minutes) spent preparing the RFA and the date of the follow-up appointment with the patient. Time to specialist input was calculated as the date the RFA was sent to the eConsultant to the date of the patient’s follow-up GP appointment. Percentage of RFAs answered within three (business) days was calculated from send and receive information from the secure messaging platform. Data are presented as mean ± standard deviation (SD), or number (percentage).
An open-ended eQuestionnaire was conducted with a targeted sample of key stakeholders to give feedback on experiences with the eConsultant model, strengths and challenges, and suggestions for improvement. This involved one urban and two rural/remote GPs from separate practices, the general physician, three patients from rural/remote areas, a practice manager, a member of the Mater Digital Technology and Information Division and a member of the Western Queensland Primary Health Network (PHN) support team. The two questions are presented in Table 1.
| Table 1. Responses to open-ended questions (n = 9) |
| From your perspective, what worked well in the eConsultant project? |
| ‘… assisted us greatly in providing our patients with expert advice and appropriate management.’ [GP, rural/remote] |
| ‘… a quick turnaround … detailed responses to each clinical question significantly improved patient management … without our patients needing to travel 800 km or wait months for an appointment.’ [GP rural/remote] |
| ‘The asynchronous nature of the interaction … doing it from home.’ [Specialist physician] |
| ‘The availability of the project lead to speak with GPs was well received by stakeholders.’ [WQPHN manager] |
| ‘Fast agile project with quick decision making, flexible with technology solutions, right people with the right knowledge involved.’ [DTI Division member] |
| ‘… saved a lot of time to go to Brisbane just to see a specialist.’ [Patient, rural/remote] |
| ‘Developing a system that integrated the process into the doctors’ normal workflow. This has been further improved with the implementation of secure messaging (Medical Objects).’ [Practice manager] |
| From your perspective, what were the challenges or barriers with the eConsultant project and how did you think they could be best overcome? |
| ‘Initially there were a few IT issues; however, as I refer more patients into the program, problems with IT has been minimal.’ [GP, rural/remote] |
| ‘… the inability to send images via Medical Objects.’ [GP, rural/remote] |
| ‘Sending off a question and waiting for the reply works in some situations but usually I need to make a decision at the time of consultation, so phoning a friend is usually what happens or referring through the normal processes … I think with the way telehealth is evolving through the COVID-19 crisis, the niche for this service could become more frequently used.’ [GP, urban] |
| ‘The communication techniques initially were tricky but the medical objects is a really good platform to use.’ [Specialist physician] |
| ‘Where practices are not currently using Medical Objects to send referrals, it must be recognised that a change management strategy must be employed to transition users to a new platform, so eConsultant requests can then be transmitted.’ [WQPHN manager] |
| ‘New technology that hadn’t really been used before. Ideally look for a solution that is already in place. That being said, it was fairly easy to setup the software to meet the needs.’ [DTI Division member] |
| ‘Educating and supporting the practitioners in using the system, reminding and encouraging the practitioners to use the eConsultant. Each practice needs a “champion” who develops/understands/monitors the process.’ [Practice manager] |
| DTI, Digital Technology and Information; GP, general practitioner; IT, information technology; WQPHN, Western Queensland Primary Health Network |
Results
eConsultant patients
eConsultant access was generated for 30 patients who all met Category 1–3 OPD referral criteria. Patient characteristics, including the primary clinical problem and comorbidities, are summarised in Table 2. Patients were predominantly aged >60 years and had an average of 3.2 (SD: 2.0) comorbidities.
| Table 2. Pilot study participant characteristics (n = 30) |
| Characteristic |
Mean ± SD or n (%) |
| Age (years) |
67.1 ± 15.8 |
| Sex |
| Male |
15 (50.0) |
| Female |
15 (50.0) |
| Setting |
| Urban |
10 (33.3) |
| Rural/remote |
20 (66.7) |
| Practice (%) |
| Urban 1 |
10 (33.3) |
| Rural/remote 1 |
3 (10.0) |
| Rural/remote 2 |
14 (46.7) |
| Rural/remote 3 |
1 (3.3) |
| Rural/remote 4 |
2 (6.7) |
| Primary clinical problem of request for advice |
| General medicine/multiple |
8 (26.7) |
| Musculoskeletal |
5 (16.7) |
| Haematological |
3 (10.0) |
| Endocrine |
3 (10.0) |
| Renal |
2 (6.7) |
| Cardiovascular |
1 (3.3) |
| Hepatology |
1 (3.3) |
| Respiratory |
1 (3.3) |
| Neurology |
1 (3.3) |
| Other* |
5 (16.7) |
| Comorbidities |
| 0 |
3 |
| 1–2 |
11 |
| ≥3 |
16 |
*Includes ear, nose and throat; urology; gynaecology and surgery
SD, standard deviation |
Outcome data are presented in Table 3. The majority (n = 23, 76.7%) of RFAs were answered within three business days (mean time: 2.1 days, SD: 1.2). with only 13.3% (n = 4) recommended for a face-to-face OPD appointment. On three occasions a specific question was not asked with the RFA and required follow-up (n = 3). RFAs mostly related to management or monitoring of chronic conditions, with 50% (n = 15) including multiple questions. More information/clinical clarification was required by the physician from the GP in 13.3% (n = 4) of cases; in all cases the GP replied in fewer than three days, and the mean additional time for the physician to respond was 10 minutes (SD: 0.0).
| Table 3. Pilot study outcomes (n = 30) |
| Outcome |
Mean ± SD or n (%) |
| Time |
| From GP RFA to eConsultant reply (days)* |
2.1 (1.2) |
| For patient to receive specialist input (days)† |
14.8 (16.7) |
| GP to generate RFA (minutes)‡ |
14.3 ± 5.6 |
| Specialist to generate reply to RFA (minutes) |
26.9 ± 19.0 |
| Recommended for face-to-face OPD visit |
4 (13.3) |
| RFAs required further information/clinical clarification |
4 (13.3) |
| RFA not appropriate for general medicine |
2 (6.7) |
| Specialist requested a more specific question from GP |
3 (10.0) |
| Type of eConsultant question§ |
| Diagnosis |
12 |
| Management |
19 |
| Monitoring |
15 |
| Other |
3 |
*Calculated on the basis of number of business days. Excluded n = 2 delay in messaging receipt at the Mater >72 hours, n = 1 prior to trial commencement
†The date the RFA was sent to the eConsultant to the date of the follow-up GP appointment with the patient; missing data n = 1
‡Missing data n = 8
§Diagnosis (eg interpretation of diagnostic testing; guidance with choosing appropriate test); management (starting, changing or ceasing a medication; conditions for starting treatment, consider other specialty consult; discuss adverse effects of medication, medication interactions); monitoring (appropriate interval for screening tests; symptom monitoring only).
GP, general practitioner; OPD, outpatient department; RFA, request for advice; SD, standard deviation |
Stakeholder eQuestionnaires
eQuestionnaires were completed by all seven delivery stakeholders and two of the three patients. Responses are summarised in Table 1.
Discussion
This pilot study shows the potential for implementation of an internationally validated model of care, with benefits to Queensland patients, practices and the health system.
Timeliness
The mean time for general physician–to–GP reply via secure messaging was 2.1 days, and where additional information was required by the physician, the GP response was timely. The mean turnaround time for patients to discuss the specialist advice with their GPs (14.8 days) was 15 days less than Category 1, 75 days less than Category 2 and 350 days less than Category 3 recommended waiting list timeframes.22 In addition, the eConsultant mean time to assess the RFA and respond via secure messaging was 27 minutes, well below the 45–60-minute OPD appointment booking usually allocated for new patient assessments.
Access
All RFAs received an answer from the eConsultant. In 87% of cases, patients avoided a face-to-face specialist visit, with the associated savings in cost and time for travel particularly noted by patients and providers in rural/remote areas. The majority of patients had three or more comorbidities, with RFAs largely focused on disease management or monitoring. This reflects the growing number of patients within general practice with complex comorbidity, and the challenge faced by GPs in adjusting medication and maintaining or fine-tuning management.
Quality
All RFAs were judged by the general physician to meet Category 1–3 OPD criteria, with the majority classified as Category 3. In all cases, RFAs were accompanied by an auditable record, in Medical Objects, of the interaction between the GP and specialist in both practice and hospital settings, avoiding the risks of the unrecorded ‘curbside’ phone conversations often used by GPs for contemporaneous specialist advice.23 All episodes were completed with the patient follow-up visit, with neither the GP nor eConsultant noting any quality or safety concerns.
Practice capacity building and support
Practices varied in their internal ability to create the required templates, and processes that were specific to their organisational needs and software systems. However, partnership between the PHN practice support staff and the research team allowed all practices to establish and maintain effective messaging and software infrastructure for the study. The method of secure messaging employed meant that any practice software with the appropriate enablement could speak to the eConsultant.
Workforce
The RFA process is designed to follow as closely as possible the GP’s usual practice for secondary care support. The RFA template mirrors the clinical information summary that is usually created via the practice software for an OPD referral, but it is prefixed by a focused question/s that the GP needs answered by the eConsultant for ongoing management of the patient. GPs documented a mean time of 14.3 minutes to generate and send the RFA. It is expected that this time will reduce as GPs become more familiar with preparing RFAs. In addition, the quality and clarity of the RFA is important if face-to-face OPD visits are to be avoided, potentially reducing concomitant health system costs. The subsequent follow-up appointment to discuss the advice with the patient again adheres to the practice’s usual billing practice and time requirement. GPs and the consultant greatly valued the flexibility of secure messaging, allowing communication at times and in settings convenient to the doctor, rather than within the strict timeframes of the physical workplace. The present study highlighted potential workforce benefits for physicians, including increased workplace flexibility and variety.24
Perceptions of the model
GPs and patients valued the timely, effective specialist input enabled by the eConsultant model of care, as well as the relative technical ease, incorporation into the practice workflow, and continuity of patient and practice care. The eQuestionnaire of key stakeholders highlighted contextual factors that have influenced the delivery of eConsultant across urban and rural/remote settings, including practice leadership and staffing, support for digital technology, workflow integration and recent external events such as COVID-19.25,26 A number of potential barriers and risks were also identified. These include involvement and cooperation across multiple health settings; the change management process at practice, PHN, hospital and organisational information technology levels; and balancing face-to-face and virtual physician time. In addition, while the eConsultant position has become a fixed-term appointment at the Mater, there is a current lack of formalised activity-based funding or ‘store and forward’ reimbursement to support non-face-to-face care, and a formal funding model is required to sustain and expand its application more broadly.
Despite the small number of practices and patients involved in this pilot study, findings are similar to those described in the international literature,7 although the educational value of eConsultant for GPs, noted by other research centres, is still to be assessed locally.27 Data compiled from this pilot study are informing broader implementation and research of the eConsultant model via QePP, an ongoing partnership between the Centre for Health System Reform and Integration, the WQPHN, the Mater, Queensland Health and the Australian Digital Health Agency. The ongoing evaluation framework includes additional eConsultant specialties (eg endocrinology and ophthalmology), and to further understand treatment changes in response to the eConsultant advice,28 subsequent hospital utilisation, comparative costs with OPD face-to-face visits, quality and safety frameworks, and scalability at state and national levels.
Conclusion
This pilot study has shown the feasibility for implementation of a validated international healthcare initiative in the Australian healthcare setting. With the growth in complex chronic disease and comorbidity, as well as community ageing, the eConsultant has the capacity to play an important part in improving access for practices and their patients to specialist support. Ongoing research should explore efficiency modelling and an understanding of the implementation and infrastructure requirements of a scaled program. Further focus should also include the governance framework required to allow state- and Commonwealth-funded entities to collaborate in efficient, equitable and accessible care options for the growing number of Australians requiring specialist support. This is consistent with the national healthcare reform agreements currently in progress with the Commonwealth and state governments.29
Implications for general practice
eConsultant offers significant potential benefits in the Australian setting including:
- improved access for GPs to specialist support, especially in rural/remote areas
- reductions in delays for specialist input into patient care
- a reliable and auditable record of advice given by specialists
- improved provider-to-provider communication and continuity of care
- an opportunity for general practice capacity building and more direct partnership with specialist colleagues
- workplace flexibility.