Approximately one million Australian adults (4.1% of those aged 18 years and over) have type 2 diabetes (T2D).1 An additional one in six Australians older than 25 years are estimated to have impaired glucose tolerance (IGT) or impaired fasting glucose (IFG) that is collectively referred to as prediabetes.2–4 A staggering 67% of adults in Australia (12.5 million adults) are overweight or obese, which increases their risk of either developing T2D or experiencing more complications from T2D.1,2,5 By 2015, T2D was the 12th largest contributor to Australia’s disease burden, accounting for an estimated 2.3% ($2.7 billion) of total disease expenditure.1 Due to the anticipated rising prevalence of T2D, associated costs will continue to rise.2 The aetiology of T2D is multifactorial and includes increasing age, genetics and lifestyle factors.1,2 For example, the prevalence of T2D in adults who identify as Aboriginal and/or Torres Strait Islander is almost twice that of the general Australian population, with 7.9% or 64,100 adults self-reporting this diagnosis in 2018–19.1 Early detection of prediabetes and those at risk of developing prediabetes are key elements in reducing the progression to T2D.1,2,6
For years, fasting blood glucose (FBG) followed by a glucose tolerance test (GTT) was the standard approach used to screen and diagnose dysglycaemia, prediabetes and T2D.6,7 In 2011, the World Health Organization (WHO) recommended the use of glycated haemoglobin (HbA1c) as an alternative.8 Within five years, the WHO’s recommendation had been officially adopted in Australia.9–12 The move was supported by the Australian Government which, in late 2014, introduced new pathology item numbers to be funded through the Medicare Benefits Schedule (MBS) for HbA1c pathology tests to screen for diabetes.
Australian clinical practice guidelines for screening and managing diabetes are regularly updated. Regarding screening for T2D, little has changed since The Royal Australian College of General Practitioners (RACGP) and Diabetes Australia joint guidelines adopted the alternative HbA1c screening pathway in their 2016 edition (Table 1).10,11 Most recently, a joint position statement was published by the Australian Diabetes Educators Association, the Australian Diabetes Society, the Dietitians Association of Australia, Exercise and Sports Science Australia and the Pharmaceutical Society of Australia.12 In contrast with the RACGP guidelines, which focus on screening and diagnosing T2D in asymptomatic people, the newer guidelines apply a lower threshold when using the Australian type 2 diabetes risk assessment tool AUSDRISK13 to identify and screen for prediabetes that is defined by IFG, IGT and/or elevated HbA1c that are yet to meet the diagnostic criteria for T2D (Table 1). Both recommended FBG or HbA1c as a first-line investigation, with GTT being reserved for instances when the GTT results will influence the management of a borderline abnormal FBG result.11,12 It should also be noted the diagnostic criteria for prediabetes remains contentious due to poor correlations between the three tests, poor reproducibility in adult and paediatric populations, and possibly different underlying pathophysiology.3 Consequently, the WHO, the American Diabetes Association, the RACGP, and the Australian joint position statement all use slightly different criteria for screening and diagnosing prediabetes.4,11,12
| Table 1. Nationally recommended screening pathways for prediabetes and asymptomatic type 2 diabetes11,12 |
| |
Prediabetes |
Type 2 diabetes |
Screen every 1–5 years
|
|
|
| Screen every three years |
- Previous prediabetes screening result: FBG <6.1 mmol/L OR HbA1c <42 mmol/mol (<6.0%) and AUSDRISK score 6–11
|
- AUSDRISK score ≥12
- All people with a history of a previous cardiovascular event (acute myocardial infarction or stroke)
- Hx gestational diabetes
- Hx polycystic ovary syndrome
- Patients on antipsychotic drugs
- Previous diabetes screening result: FBG <5.5 mmol/L; FBG <6.1 mmol/L and 2-hour GTT <7.8 mmol/L; OR HbA1c
<42 mmol/mol (<6.0%)
|
| Screen every year |
- Previous prediabetes screening result: FBG <6.1 mmol/L OR HbA1c <42 mmol/mol (<6.0%) and AUSDRISK score ≥12
|
- Aboriginal and Torres Strait Islander people ≥18 years of age
- Previous diabetes screening result:
FBG 6.1–6.9 mmol/L with GTT <11.1 mmol/L; OR HbA1c 42–46 mmol/mol (6.0–6.4%)
|
| First-line screening |
FBG or HbA1c |
FBG or HbA1c (or RBG for Aboriginal
and/or Torres Strait Islander people*) |
| FBG result† |
|
|
| <5.5 mmol/L |
|
Screen in three years |
| <6.1 mmol/L |
Screen in 1–3 years |
Request GTT, screen in three years |
| 5.5–6.9 mmol/L |
|
Diabetes possible – request GTT |
| 6.1–6.9 mmol/L |
Prediabetes likely – consider GTT‡ |
IFG likely – request GTT, screen in one year |
| ≥7 mmol/L |
|
Diabetes likely – repeat FBG |
| HbA1c result |
|
|
| <42 mmol/mol (<6.0%) |
Screen in 1–3 years |
Screen in three years |
| 42–46 mmol/mol (6.0–6.4%) |
Prediabetes likely |
High risk – screen in one year |
| >46 mmol/mol (>6.4%) |
|
Diabetes likely – repeat HbA1c |
| Second-line screening |
Glucose tolerance test (GTT) |
Glucose tolerance test (GTT) |
| Two-hour GTT (75 g oral glucose dose) result |
|
|
| <7.8 mmol/L |
|
Screen in three years |
| 7.8–11.0 mmol/L |
Prediabetes likely with IGT |
IGT – screen in one year |
| ≥11.1 mmol/L |
|
Diabetes |
Note: The risk of developing T2D in the next five years is one in 50 with a score of 6–8, one in 30 with a score of 9–11, and one in 14 with a score of 12–15. The score tends to overestimate risk in people younger than 25 years and underestimate risk in Aboriginal and/or Torres Strait Islander people.10
*An RBG ≥11.1 mmol/L is suggestive of T2D.
†FBG categories overlap because of different cut offs for prediabetes guidelines12 and type 2 diabetes guidelines.11
‡GTT is indicated to differentiate between IFG and IGT to inform intensive lifestyle intervention.
AUSDRISK, Australian type 2 diabetes risk assessment tool; FBG, fasting blood glucose; GTT, glucose tolerance test; HbA1c, glycated haemoglobin; Hx: clinical history; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; RBG, random blood glucose; T2D, type 2 diabetes |
To further understand the extent to which changes to clinical practice guidelines and available pathology tests are being used in Australia to reduce progression along the T2D continuum, this study examined 10-year annual trends, from 2010–19, in the use of relevant MBS-funded T2D pathology testing by Australian doctors.
Methods
A secondary analysis was conducted of publicly available data reporting MBS pathology services for the 10 calendar years 2010–19. Relevant MBS item numbers for pathology tests were identified by searching the Australian Government MBS Online14 with the terms ‘diabetes’, ‘glucose’, ‘fasting glucose’, ‘fasting plasma glucose’, ‘glycated haemoglobin’, HbA1c, ‘Glucose tolerance test’, ‘GTT’, ‘Type 2 Diabetes’, ‘Type 2 Diabetes Mellitus’ and ‘T2D’. Eight item numbers for pathology tests that can be requested by medical practitioners and are relevant to the diagnosis and/or management of patients with diabetes and those at ‘high risk’ of developing diabetes were identified (Table 2). While insulin is currently not recommended for routine screening for prediabetes or diabetes,11,12 it was included nonetheless due to ongoing debate regarding its role in the pathogenesis of prediabetes and diabetes,15,16 and as an additional screening test for certain population groups.17,18 As such, it is likely that some medical practitioners are ordering insulin tests despite it not being routinely recommended.
| Table 2. Medicare Benefits Schedule (MBS) pathology item numbers for diagnosis or management of diabetes mellitus |
| Indications |
MBS item number |
Description |
| Screening |
66841 |
HbA1c performed for the diagnosis of diabetes in asymptomatic patients at high risk |
Screening
Aboriginal and/or Torres Strait Islander people only* |
73839 |
HbA1c performed for the diagnosis of diabetes in asymptomatic patients at high risk (not more than once in a 12-month period) |
| Screening |
66542 |
Oral glucose tolerance test with at least two measurements of glucose (plus any test described in item 66695 such as insulin) for the diagnosis of diabetes |
| Screening or management |
66500 |
Serum, plasma, urine or other body fluid (except amniotic fluid), by any method except reagent tablet or reagent strip (with or without reflectance meter) of one or more of 29 biochemical substances (eg electrolytes, urea, creatine, liver enzymes and lipids), including glucose and urinary microalbumin |
| Screening or management† |
66695 |
Quantitation in blood or urine of one or more of 27 hormones and hormone-binding proteins (eg adrenocorticotropic hormone, growth hormones, glucagon, sex hormones, urine steroid fraction or fractions), including insulin |
| Management |
66551 |
HbA1c performed in the management of established diabetes |
Management
Aboriginal and/or Torres Strait Islander people only* |
73840 |
HbA1c performed in the management of established diabetes (maximum of four tests in a 12-month period) |
Management
Aboriginal and/or Torres Strait Islander people only* |
73844 |
Urinary microalbumin from a timed overnight urine sample or urine albumin:creatinine ratio as determined on a first morning urine sample in the management of established diabetes |
*Quality Assurance in Aboriginal Medical Services (QAAMS) Program items
†Insulin and other hormones are currently not recommended for routine screening for prediabetes or diabetes.
HbA1c, glycated haemoglobin; MBS, Medicare Benefits Schedule |
Annual service data for the eight MBS item numbers (66841, 73839, 66542, 66500, 66695, 66551, 73840 and 73844) were downloaded from the Medicare Statistics – Services Australia website.19 The data represent those services performed by a registered pathology provider that qualifies for a Medicare payment and for which a claim has been processed by Medicare Australia. This represents the bulk of primary care services where most of the routine screening for T2D takes place. It does not include services provided by hospitals to public patients in public hospitals or services that qualify for a benefit under the Department of Veterans’ Affairs National Treatment Account.20 Given that the pathology services of greatest interest for this study are mostly provided in community rather than hospital settings and, therefore, mostly funded through the MBS, for pragmatic reasons, no other data sources were sought.
Microsoft Excel was used to generate summary tables and charts. Data for the general Australian population and the Quality Assurance in Aboriginal Medical Services (QAAMS) Program item numbers were extracted for the number of services and as rates per 100,000 according to age groups and sex for the calendar years 2010–19. The decision to compare calendar years rather than financial years reflected anecdotal reports that chronic disease management, including ongoing pathology referrals and screening, had suddenly dropped due to the COVID-19 pandemic. For the sake of brevity, the data are presented as figures. Supporting tables with detailed information are available upon request.
Human Research Ethics Committee approval was not required as all data used in the analysis were de-identified and publicly available.
Results
Across the 10-year period of 2010–19, a number of changes in the rates and types of pathology tests provided to diagnose diabetes were observed (Figure 1). An average of 1105 GTTs per 100,000 persons (MBS item no. 66542) were provided each year to diagnose diabetes. These rates were steady until 2015, when they started to decline. This correlated with the introduction of HbA1c (MBS item nos 66841 and 73839) as an alternative diagnostic test. By the end of 2019, the rate of GTT services provided each year had halved from 1333/100,000 persons in 2010 to 687/100,000 persons in 2019, and HbA1c diagnostic services had increased from 926/100,000 persons in 2015 to 2076/100,000 persons in 2019. Combined, the rate of diabetes screening tests conducted each year had doubled over the 10-year period.
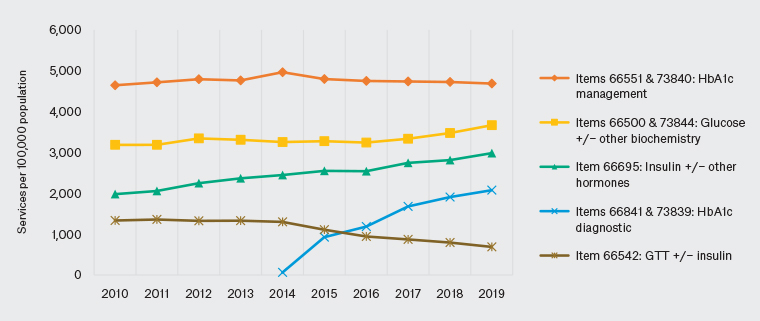
Figure 1. Medicare Benefit Schedule diabetes-related pathology services for the general Australian population
HbA1c, glycated haemoglobin; GTT, glucose tolerance test
In contrast, the use of HbA1c for the ongoing management of diabetes (MBS item nos 66551 and 73840) remained relatively unchanged before and after the introduction of MBS funding for HbA1c tests to diagnose diabetes (Figure 1). Across the 10 years, an average of 4758 services per 100,000 persons were provided each year. Notably, this was substantially higher than any of the other pathology tests reviewed, including general biochemistry tests with or without glucose (MBS item nos 66500 and 73844) and general hormonal tests, with or without insulin (MBS item no. 66695).
Diabetes screening differed according to age, sex and Indigenous status (Figure 2). For instance, based on the latest figures from 2019, the rate of GTT (MBS item no. 66542) was 1.7 times higher for females (873/100,000 females) compared to males (499/100,000 males). For females, the largest proportion were provided to those aged 25–44 years (44%). This equated to one-third of the total number of GTT services (59,595/175,967 GTT services). For males, the largest proportion were provided to those aged 55–74 years (49%). However, the total number of services provided was only slightly higher for males aged 55–74 years compared to females (males 33,799/175,967 GTT services, 19.2%; females 29,594/175,967 GTT services, 16.7%).
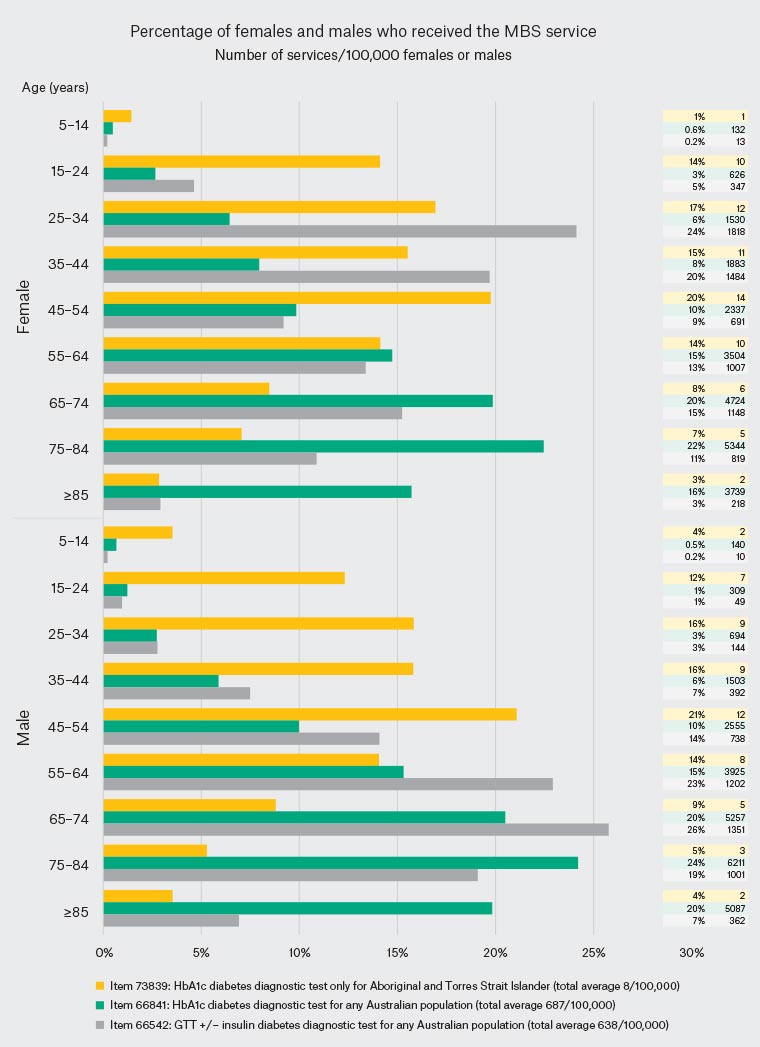
Figure 2. Demographic characteristics of Medicare Benefit Schedule (MBS) diabetes diagnostic pathology services in 2019. Click here to enlarge.
HbA1c, glycated haemoglobin; GTT, glucose tolerance test
Substantial differences were also observed in the age at which the HbA1c diagnostic tests were provided to people who identify as Aboriginal and/or Torres Strait Islander (MBS item no. 73839) compared to the general Australian population (MBS item no. 66841; Figure 2). A higher proportion (32%) of the HbA1c diagnostic tests were provided to both male and female adolescents and younger adults aged 15–34 years who identify as Aboriginal and/or Torres Strait Islander (MBS item no. 73839). From age 55 years, the proportion of people being tested started to decline, with less than 20% of tests being provided to adults older than 64 years. In sharp contrast, for the other HbA1c diagnostic test that can be used by anyone (MBS item no. 66841), less than 10% of tests were provided to people under the age of 35 years. Over 60% of HbA1c diagnostic tests (MBS item no. 66841) were provided to adults older than 64 years.
Discussion
This study identified a number of trends in the MBS pathology service provided to Australians for the diagnosis and management of diabetes. There was evidence of a strong adoption of national diabetes guidelines. HbA1c was increasingly being used to screen for T2D in high-risk adults, including younger adults who identify as Aboriginal and/or Torres Strait Islander. A large proportion of younger females in the reproductive age groups were referred for GTT.
Over the 10-year period, screening rates for diabetes in Australia had doubled. While this is commendable as it suggests healthcare practitioners are proactive, it is also concerning as it highlights that, 10 years on, so many Australians meet the screening criteria and have a high risk of developing T2D. Notably, adults who identify as Aboriginal and/or Torres Strait Islander were being screened at a much younger age, highlighting the disparity in their increased risk of developing T2D compared to the general Australian adult population.1 While the available MBS data were unable to differentiate the reasons for GTT, it is quite likely that a large number of females in the reproductive age groups are being screened for gestational diabetes and/or polycystic ovarian syndrome, both of which are associated with an increased risk of developing T2D.11,18 These trends in HbA1c and GTT testing further affirm the importance of evidence-based lifestyle interventions at both the individual and population/community levels to help reverse the otherwise likely progression to T2D and its sequalae.2,6,9–11,19,20
The rapid rise in HbA1c services for diabetes screening, and simultaneous decline in GTT services following the introduction of MBS HbA1c screening items in 2015, is also noteworthy. It is unclear the extent to which the original screening pathway that begins with an FBG, followed by GTT if indicated, is still being performed, or how often FBG is being tested alongside HbA1c and how this might impact clinical decisions and MBS costs. National guidelines do not state a preference; either test is acceptable.11 Patient and provider preferences are therefore likely to be influencing these trends. From the patient’s perspective, HbA1c testing does not require fasting and there are no additional tests for borderline results suggestive of prediabetes (HbA1c 42–46 mmol/mol [6.0–6.4%]). Conversely, the person must fast before an initial FBG screening test, and borderline results (5.5–6.9 mmol/L) are referred for a GTT that is also a fasting test, which takes at least two hours to complete and involves multiple venesections. From the provider’s perspective, only the HbA1c screening test attracts primary care Service Incentive Payments and Practice Incentive Payments. Conversely, an additional MBS payment for a consultation with a medical practitioner is likely for borderline FBG results. Further information about patient and provider preferences, along with an analysis of the cost-effectiveness of the recommended screening pathways, would help guide patient-centred diabetes care and value-based decision making and policies.20–22
Regarding screening and management for prediabetes, Table 1 highlights potential confusions that are likely to arise for Australian practitioners and patients due to different cut-offs and screening intervals for the same test.10,11 Further, diabetes screening pathways begin with either an FBG or HbA1c; however, neither test is ideal for screening for prediabetes. For example, in a meta-analysis of 46 studies that used GTT as the gold standard for defining prediabetes, the pooled sensitivity and specificity of HbA1c was 49% and 79%, respectively.22 For FBG, the sensitivity was only 25%; however, specificity was much higher, at 94%.22 In another meta-analysis that pooled the individual data from 16 studies, the most optimal prediabetes cut-off levels for predicting the risk of developing T2D within the next five years were calculated to be 5.6 mmol/L for FBG (sensitivity 64%, specificity 77%), 38 mmol/mol (5.6%) for HbA1c (sensitivity 73%, specificity 80%) and 7.0–11.1 mmol/L for two-hour GTT (sensitivity 62%, specificity 81%).4 Lower cut-off levels were also evaluated but these did not significantly improve the overall predictive accuracy, as the trade-off for a higher sensitivity was lower specificity. The reproducibility of FBG and HbA1c also tends to be lower for people with prediabetes, at approximately 50%, compared to 70% for people with T2D.3
MBS data were unable to determine the extent to which medical practitioners might be using other tests, such as fasting glucose and insulin. Australian guidelines do not discuss the use of fasting insulin, either as a standalone test or as part of a GTT.11,12 However, there are a number of reasons why it is likely that at least some insulin tests might be used by Australian doctors to screen for prediabetes and diabetes. The low sensitivity and specificity of FBG and HbA1c, especially in adolescents and young adults, have prompted calls to check fasting insulin in these population groups before subjecting patients to a GTT.16 Although currently not recommended,23 fasting insulin is also used by some clinicians to identify high-risk females with polycystic ovarian syndrome.18 The role of hyperinsulinemia, rather than insulin resistance, is increasingly being postulated as the underlying driver of the metabolic syndrome, prediabetes and T2D.15,16 Evidence is also mounting to suggest that elevated fasting insulin is correlated with early cardiometabolic derangements independent of insulin resistance or hyperglycaemia.15 While more research is needed, this raises the question as to whether a new insulin-specific MBS item number is warranted, particularly if fasting insulin is found to be an early, cost-effective risk identifier.
Limitations of this study included only analysing MBS data. Pathology services provided and funded by state and territory secondary care services, Department of Veterans’ Affairs-funded services and privately funded services were excluded. The nature of the available MBS data was another limitation. It is quite likely that some of the HbA1c tests were miscoded, as the pathology providers rely upon the information on the request form to determine which MBS item number applies. Also, it was not possible to determine which medical practitioner, general practitioner (GP) or secondary care specialist had ordered the pathology tests. Notwithstanding, MBS data reflect the majority of referrals made by GPs and other primary care providers, who are the backbone of diabetes screening in Australia. The scope of the MBS item numbers for fasting glucose and insulin were non-specific, which in turn prevented any detailed analysis of pathology referral patterns. Similarly, a more specific analysis would have been possible if the other MBS item numbers had more specific indications (eg different MBS item numbers for GTT to screen for gestational diabetes and T2D).
Conclusion
Analysis of 10 years of MBS pathology services for the diagnosis and management of T2D reflected changes to Australian recommendations for diabetes screening. Ongoing research is needed to monitor the impact of these recommended screening pathways, particularly for the early detection of prediabetes and to identify opportunities for further cost savings and disease prevention. To this end, greater reconciliation of prediabetes and T2D screening pathways is required, along with more information about provider and patient perspectives, particularly adolescents and young adults, older adults, and people from culturally and linguistically diverse backgrounds.