Approximately 77% of individuals living in the residential aged care sector (RACS; ie nursing homes) following stroke have upper limb spasticity and experience pain and significant passive care difficulties.1 Palmar ulceration caused by spastic fingers is an under-recognised complication of upper limb post-stroke spasticity (PSS). These ulcerations can be painful, emit offensive smell and cause significant suffering for the individuals, their families and the carers. There is an unmet need for management of spasticity and its complications in the RACS.1 A substantial number of patients with significant impairments following stroke are placed in the RACS. Currently there is no structured multidisciplinary spasticity management program for the management of spasticity in the RACS. Research has shown that complications such as palmar ulcerations in the spastic hand can be mitigated by reducing spasticity in the hand using botulinum toxin A (BoNTA) injection followed by dressing, splinting and therapy.2,3 A group of patients living in the RACS with post-stroke spasticity developed hand ulcerations and were treated in a spasticity clinic at a tertiary hospital. The methods of treating these patients and the results of the treatment outcomes have been published previously.3 In this review article, we discuss the epidemiology, anatomy and different clinical presentations of the spastic hand, along with the mechanisms of action of BoNTA in alleviating ulcers and related symptoms such as pain and sweating, leading to significant improvement in patient outcomes and lessening of carer burden. The primary objective of this article is to alert general practitioners and other physicians to this complex problem and the appropriate management.
Epidemiology of upper limb PSS in the RACS
There is a paucity of data regarding the prevalence and management of spasticity among individuals residing in the RACS.4,5 Stroke is one of the common causes of spasticity and is reported to be present in 22% of residents examined by a neurologist.6 In a study conducted in the USA and UK, approximately 15–18% of nursing home residents >65 years have had a stroke. The study also reported that PSS is underdiagnosed and inadequately treated in individuals living in the RACS.7 In an Australian study,8 researchers found 19.3% of all individuals living in the Australian RACS had previously had a stroke. The same group reported that approximately 70% of individuals living in the RACS with a history of stroke had upper limb spasticity. This study also found upper limb PSS was associated with pain and significant passive care difficulties. The prevalence data are similar to results from a cross-sectional study performed by Meijer et al, reporting spasticity among 73% of a mixed cohort of patients with central nervous system disorders in a nursing home. Individuals with past ischaemic stroke constituted the most common group. Meijer et al studied a population group of 850 patients in three nursing homes.9
PSS and the hand
The human hand has a complex anatomy, and it is instrumental in multiple grips and postures resulting from highly mobile fingers and thumb.10 The hand is a multipurpose body part involved in reaching, grasping, manipulating objects and feeling. It is also an important conduit to our rich tactile and communicating world.11 The evolution of human hand dexterity became possible to a significant extent because of the highly mobile thumb.12
PSS commonly affects the hand; the thumb loses its mobility and gets drawn into the palm in what is known as the thumb-in-hand deformity, and the fingers flex unbidden as a result of the hyperexcitability of stretch reflexes, giving rise to a permanently clenched fist. The hand is no longer capable of conducting active tasks such as feeding, dressing, grooming and other activities of daily living. Moreover, individuals with unmitigated upper limb spasticity develop pain, deformity, contracture and, in some cases, serious complications such as palmar ulcerations in the hand. Family members and carers find it exceedingly difficult to clean the individual’s hands and maintain hand hygiene.1,2
Besides stroke, individuals with upper motor neurological disorders such as brain injury, multiple sclerosis and cerebral palsy are also vulnerable to develop similar conditions.
Functional anatomy and clinical presentation
PSS in the upper limb manifests as clenched fist, flexed wrist and pronated forearm. The elbow is flexed, and the shoulder joint remains adducted and internally rotated.
The clenched fist is due to spasticity in the spastic flexor digitorum superficialis and flexor digitorum profundus muscles. The thumb-in-hand deformity is caused by spastic flexor pollicis longus, flexor pollicis brevis, adductor pollicis and the first dorsal interosseus muscles.2 Intrinsic plus hand deformity is caused by spastic lumbricals and interossei muscles. Wrist flexion is due to spastic flexor carpi ulnaris and flexor carpi radialis muscles, with secondary contribution from the long finger flexors. Forearm pronation is caused by spasticity in the pronator teres and pronator quadratus muscle. These specific muscles causing various deformities, and the objective assessment of the spastic hand pre- and post-BoNTA injection have been described elsewhere.2
Pathophysiology of palmar ulceration due to hand PSS
Spasticity is the most common cause of difficult-to-treat pressure ulcers in atypical locations, such as the hand.13,14 In the spastic hand, fingers can neither be actively nor passively extended to facilitate cleaning of the hand.13,14 In some cases, the spastic and distorted fingers, often with overgrown nails, press unremittingly into the palm. It is recognised that ‘external pressure of more than 33 mmHg occludes capillary perfusion so that the underlying and surrounding tissues become anoxic and if the pressure continues for a critical duration, cell death will occur, resulting in soft tissue necrosis and eventual ulceration’.15 Over time, pressure from the spastic fingers with overgrown nails causes skin breakdown,16 resulting in atypical pressure ulceration in the palm of the hand, commonly around the proximal palmar, distal palmar and metacarpophalangeal creases. It becomes difficult to dress these ulcers and maintain general cleanliness and hygiene because the hand cannot be opened. These painful and apparently untreatable ulcers of the hand and fingers cause intense suffering for the patient and stress for families and carers. Spasticity thus creates a powerful barrier as the ulcers become inaccessible to treatment.17 Ulcerations are more common on the ulnar side of the hand (Figure 1A and 1B). It is reported that the ulnar two digits play a significant part in hand grip. The overall grip strength decreases to 34–67% (with a mean decrease of 55%) without the contribution of the ulnar digits.18 It is hypothesised that the stronger ulnar flexor muscles become more spastic than the muscles on the radial side, giving rise to ulcerations occurring commonly on the ulnar side of the hand. In the wrist, flexor carpi ulnaris is the commonly deforming force and, coupled with weak extensors and radial deviators, causes wrist flexion and ulnar deviation.19
There is excessive sweating in the spastic hand (hyperhidrosis),20 which remains closed most of the time. Hyperhidrosis is the result of sympathetic hyperactivity of eccrine sweat glands in the palms. It is common for the untreated spastic hand to build up debris and become foul smelling from excessive sweating1,2 because of biotransformation of odourless natural secretions into odorous molecules (bromhidrosis).21
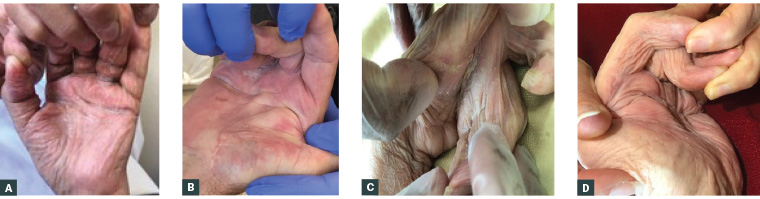
Figure 1. Examples of spastic hand with complications successfully treated
A. Pressure ulcerations in the proximal and distal palmar creases and metacarpophalangeal crease of the ring finger caused by spasticity in the flexor digitorum superficialis and flexor digitorum profundus muscles; B. Hand ulcerations involving the distal palmar crease and metacarpophalangeal crease of the ring and middle finger caused by spasticity in the flexor digitorum superficialis muscle; C. A spastic hand with longstanding finger flexion deformity and excessive sweating causing build-up of debris and ulceration underneath; D. Significant improvement following treatment with botulinum toxin A injection into the spastic hand muscles followed by dressing, splinting and therapy.
Mechanisms of BoNTA action in the healing of hand ulcerations and associated symptoms
BoNTA is useful in many disorders of the hand, such as spasticity, dystonia, hyperhidrosis, tremor and Raynaud’s phenomenon.22 Interestingly, several mechanisms of BoNTA are likely to be operational in the healing of hand ulcerations.
Injection of the toxin relaxes the spastic muscles by blocking the presynaptic release of neuromuscular transmitter acetylcholine and deactivating soluble N-ethylmaleimide-sensitive factor attachment protein receptor (SNARE) protein.23 This facilitates opening of the hand, which allows dressing and maintenance of hygiene.
BoNTA also inhibits excessive sweating by blocking the release of acetylcholine in the postganglionic sympathetic fibres to the eccrine glands, which are responsive to cholinergic stimulation, unlike the apocrine glands. Studies have shown that BoNTA is used to inhibit palmar hyperhidrosis.20,21 Reduction of palmar sweating is helpful in lessening the build-up of debris and alleviating the offensive smell. This makes it easier to dress these wounds and promotes healing of the wounds (Figure 2).
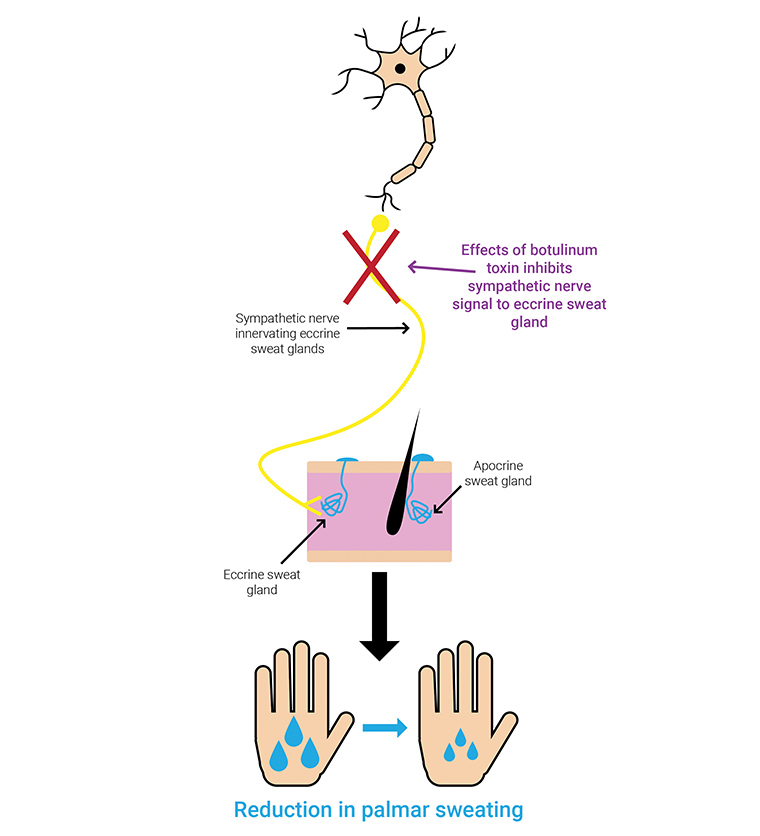
Figure 2. Mechanism of botulinum toxin A injection in relieving palmar hyperhidrosis: the toxin inhibits the sympathetic nerve signal to eccrine sweat glands.
BoNTA has been shown to be effective in vasospastic conditions such as Raynaud’s phenomenon by relieving pain and improving perfusion. The mechanism of its function is not fully elucidated. The putative mechanisms are inhibition of the activity of sympathetic and sensory nerves, inhibition of signal transduction pathways, depletion of pain mediators and vasodilatation caused by the paralysis of the acetylcholine-mediated arterial muscles (Figure 3).
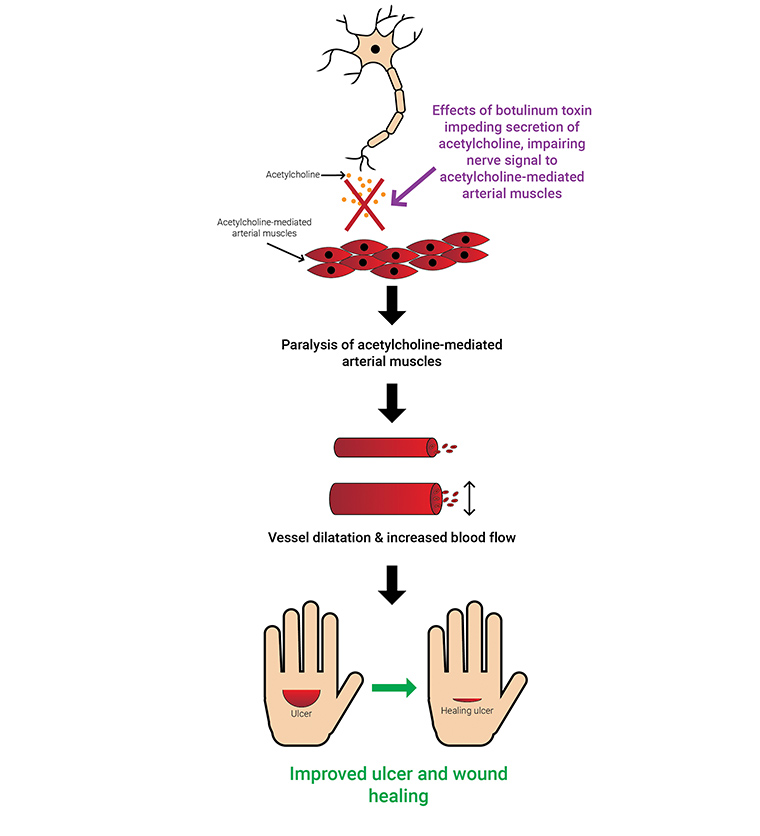
Figure 3. Mechanism of botulinum toxin A in improving circulation: inhibition of sympathetic adrenergic or cholinergic vasoconstriction, inhibition of sensory nerves and/or endothelial exocytosis of endothelin 1, and inhibition of pain that causes vasodilatation, helping to heal the ulcerations.
The possible mechanisms of BoNTA on relief of pain involve 1) retrograde axonal transport of toxin, 2) inhibition of neuropeptides such as substance P, calcitonin gene-related protein and glutamate (pain mediators) and 3) deactivation of sodium channels. These mechanisms of action reduce peripheral and central sensitisation (Figure 4).24
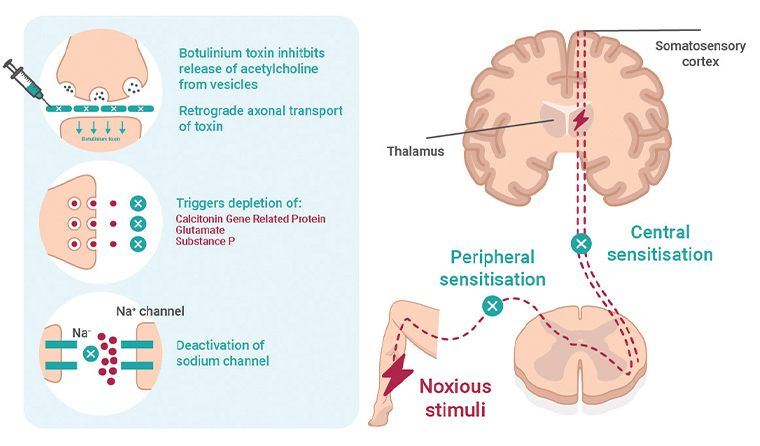
Figure 4. Mechanism of botulinum toxin A injection in pain reduction involves 1) retrograde axonal transport of toxin, 2) inhibition of neuropeptides such as substance P, calcitonin gene-related protein and glutamate and 3) deactivation of sodium channels. These mechanisms of action reduce peripheral and central sensitisation.
The BoNTA injection contributes to healing of the ulcers by the aforementioned mechanisms.25,26
BoNTA exerts its effect in 7–8 days and can last up to four months.2 The ideal candidate for treatment with BoNTA is an individual who is developing a closed fist because of spasticity of the hand muscle.
Injection of BoNTA is a safe intervention with no significant side effects. The contraindications are few and include fracture or arthritis; evidence of fixed contracture; significant illness, such as malignancy; or allergy to botulinum toxin.
The deformity and ulceration may return when the hand can no longer be opened for dressing or maintenance of hygiene because of return of spasticity. This happens approximately 4–5 months post injection, when the effects of BoNTA tend to wear off. Repeat injection followed by dressing, splinting and hand therapy is needed to prevent recurrence.
BoNTA is unlikely to be effective if the muscles develop contracture. One way of determining whether contracture has occurred is to try passive movement. If the joint can be moved by passive stretching, it is indicative of spasticity. If the joint is in a fixed position and is difficult to move, it is likely to be contracted. Surgical release of contracture is the next step to open the hand, which will then allow dressing of the ulcerations.2
Conclusion
PSS is common among residents living in the RACS. As there is no multidisciplinary management of spasticity in the RACS, the residents are prone to develop palmar ulcerations as a complication of unmitigated spasticity of the hand muscles. BoNTA injection into the spastic hand muscles – along with other adjuvant measures such as dressing, splinting and therapy – can alleviate the distressing complications of hand ulcerations. BoNTA is also useful in the treatment of other symptoms related to the ulcerations, such as pain, sweating and offensive smell. The injection of BoNTA into spastic muscles followed by dressing, splinting and therapy improves patient outcomes and lessens the carer burden.3,17 Patients in the RACS who are likely to develop spasticity-related complications should be referred early to a multidisciplinary spasticity clinic in tertiary hospitals.