Injuries to the eye are a common presentation in the general practice setting.1 Prevention of permanent vision loss from eye injuries requires accurate initial assessment and early diagnosis, including good primary ocular first aid and prompt referral of serious eye injuries to an emergency department with access to an ophthalmology service. It is estimated that 90% of ocular trauma is preventable.2 Among adults, road traffic accidents are the most common causative factor, followed by assault and falls.1 In contrast, sports-related injuries account for 27% of all ocular trauma in children requiring hospitalisation.2
The modified Birmingham Eye Trauma Terminology (BETT) classification (Figure 1) should be used to ensure language is consistent when describing mechanical eye and periocular injuries across general practice, emergency departments and ophthalmology services.2,3 The original BETT classification system defined ocular injuries as a closed or open globe without reference to accompanying periocular injuries.4–6 The modified BETT classification overcomes this globe bias by incorporating extraocular injuries with or without retained foreign bodies.3 In Australia, open globe injuries account for 44% of the cost of ocular trauma services.2 Causes of ocular injuries vary according to the patient’s age and occupation. One study observed a peak incidence of open globe injuries in teenagers and young adults.7 Despite significant visual improvement following appropriate treatment, significant visual loss may still occur. Thus, the role of effective prevention in the general practice setting, along with a multidisciplinary team approach with timely and prompt ophthalmology referral, should be emphasised.
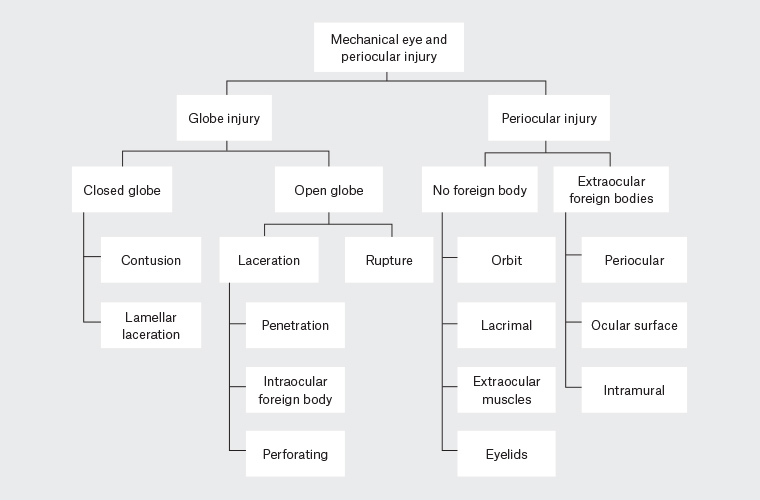
Figure 1. A modified Birmingham Eye Trauma Terminology (BETT) classification system that incorporates both globe and periocular injuries. The original BETT classification did not consider periocular injuries.
Corneal and conjunctival foreign body
History
For ocular surface foreign bodies, it is essential to know the velocity at which the object was travelling towards the eye, as this may alert the need for detailed intraocular examination to exclude penetration. The type of object that caused the injury and the timing may provide a clue to the risk and microbial spectrum of secondary infection. For example, plant matter may raise suspicion of possible fungal involvement.
Examination
Visual acuity should be measured after adequate topical anaesthesia (2–3 drops of oxybuprocaine 0.4%) to reduce reflex tearing and allow the eye to stay open long enough for testing and examination. Corneal foreign bodies can be visualised with a loop in a well-illuminated area or preferably with a slit lamp so that the depth of the object within the cornea can be assessed accurately. The Royal Australian College of General Practitioners’ (RACGP’s) curriculum includes ‘the removal of a foreign body, including any residual corneal ulcer or rust’ as a required skill.8 The presence of white infiltrate or anterior chamber reaction should be noted, as this may indicate secondary bacterial infection. Fluorescein staining will help direct the clinician to the epithelial defect, which typically surrounds the site of impact of the foreign body.8,9 It is important to evert the upper lids and sweep/irrigate for a residual tarsal foreign body that may have migrated from the cornea and may have been missed on the initial examination.
Management
After providing a few drops of oxybuprocaine to the affected eye, removal of the foreign body involves the use of a wet (sterile saline) cotton bud or 25G 16 mm hypodermic needle to pick up loose foreign body that is not embedded into the corneal stroma. Deeper foreign body may require a needle to lift the material and any associated rust ring off the base of the superficial stromal defect. After removal, concentrated fluorescein should be applied to the wound to ensure a negative Seidel test if the foreign body was removed from deep corneal stroma. The Siedel test involves the instillation of fluorescein eye drops on the ocular surface to demonstrate full-thickness corneal defects as the aqueous washes away the green dye as it emerges from the open wound, indicating a penetrating eye injury. Corneal epithelial defects and prolapsed vitreous stain green with fluorescein. Chloramphenicol ointment is applied immediately and then four times per day. Follow-up examination 1–3 days after treatment is essential to ensure the epithelial defect is resolving and that there is improvement in visual acuity and absence of secondary infection. If a corneal infiltrate develops, the patient will require urgent referral to the nearest ophthalmology service. Similarly, if the foreign body lies on the central visual axis, the patient should be referred on to an ophthalmic specialist where possible. Chloramphenicol ointment may be prescribed to those patients with difficult-to-remove corneal foreign bodies delaying complete removal by 24–48 hours following the initial presentation. Non-impaled conjunctival foreign bodies should be removed using irrigation and wet cotton buds. There is evidence to support a difference in time to healing with patching.8 Visual loss and a conjunctival defect with significant subconjunctival haemorrhage in a patient with an apparent superficial conjunctival foreign body should alert the clinician to the possibility of intraocular penetration.
Chemical eye injury
History
It is essential to elicit the type of substance and its contact time with the eye. The most serious injuries involve alkali and hydrofluoric acid burns. In general, alkali chemicals such as ammonium hydroxide (fertiliser), sodium hydroxide (caustic soda) and calcium hydroxide (lime) cause more severe injuries than those with a low pH such as sulphuric acid (car battery), sulphurous acid (bleach) and hydrochloric acid (swimming pool cleaning agents).
Examination
Chemical burns may affect the eyelids, conjunctiva and cornea. Examination should be deferred until completion of copious irrigation with normal saline or sterile water after instillation of topical anaesthetic if readily accessible. Irrigation should continue until the pH of the ocular surface has normalised to between 7.0 and 7.2. In the absence of dedicated anaesthetic eye drops (eg proxymetacaine, oxybuprocaine or amethocaine), a few drops of 1–2% lignocaine typically used for subcutaneous infiltration can also be used on the eye. The upper and lower eyelids should be everted and both the upper and lower fornices examined and swept for particulate matter. After immediate and extensive irrigation of the ocular surface, fluorescein should be instilled to assess for the presence and extent of corneal and conjunctival epithelial defects. A corneal epithelial defect that extends across the corneo-limbal junction should raise suspicion of a limbal injury. Signs of limbal ischaemia (loss of limbal blood vessels) and corneal opacity should be noted.10,11 Severe injury to the limbus results in the loss of corneal limbal stem cells, which are critical for repair of the corneal epithelial defect. Extensive loss of conjunctival epithelium in the fornix may also result in shortening of conjunctiva (symblepharon) and lid malposition.
Management
Irrigation should be commenced immediately with no delay using normal saline (2 L) or sterile water. Topical anaesthesia may be applied simultaneously to enable adequate exposure of the ocular surface to the wash. The patient should, where possible, be positioned supine while saline is poured into the injured eye for at least 15 minutes. The pH can then be assessed using litmus paper. Additional irrigation is required until the pH is 7.0–7.5. Any patient with limbal ischaemia (whitening) or corneal opacities should be urgently referred for tertiary ophthalmic management following appropriate irrigation. The pH should be compared with the other eye. An eye pad should not be placed over the eye as this may lead to a de-epithelialised cornea.10
Orbital fracture
History
For patients presenting with a suspected orbital fracture, it is essential to ask about diplopia and pain on eye movements. Visual loss may indicate concurrent globe or optic nerve injury. The size or nature of the object that struck the eye socket can provide an indication of whether the globe has been pushed inward to cause a blowout fracture or if the orbital rim received the maximal impact, with the transmitting force fracturing the orbital wall directly. It may also raise suspicion for a penetrating eye injury.
Examination
An initial assessment of the patient’s neurological status should be performed to exclude an intracranial injury. The examiner should then test for a relative afferent pupillary defect (RAPD) to determine optic nerve function, as evidence of an optic neuropathy calls for expedited neuroimaging to exclude a compressive or crush injury to the optic nerve.12 The next step is to observe for the presence of proptosis or enophthalmos. The orbital rim should be palpated for discontinuity and detachment of the medial canthal tendon; both are signs of severe orbital trauma. Globe integrity and ocular motility should be documented, as well as a neurological examination of the V1 and V2 branches of the trigeminal nerve, which may be affected by an orbital roof and floor fracture, respectively. If trismus is present, an underlying zygomatic maxillary complex fracture may be present. Severe upward gaze restriction with pain, nausea, syncope and/or bradycardia (oculocardiac reflex) may indicate entrapment of the inferior rectus.
Management
Patients with an RAPD, reduced vision, proptosis or severe entrapment syndrome (absent upward gaze with pain and oculocardiac reflex) should be referred urgently to an ophthalmology or maxillofacial service for further assessment and surgery.13,14 Orbital decompression with a lateral canthotomy may be required in cases of retrobulbar haemorrhage compromising optic nerve function. Urgent repair of the fractured orbital wall/floor to release entrapment of the medial or inferior rectus and orbital tissue can prevent ischaemia, fibrosis and haemodynamic instability secondary to the oculocardiac reflex.13,14 The patient should be told to avoid blowing their nose. Isolated orbital floor fractures are indicated for immediate repair when there is diplopia with computed tomography (CT) evidence of entrapped muscle or periorbital tissue associated with a persistent oculocardiac reflex.15 In those <18 years of age with a history of periocular trauma, marked extraocular motility vertical restriction and a white eye, a ‘white-eye blowout fracture’ should be considered. Immediate repair is indicated if CT confirms an orbital floor fracture with entrapped muscle or perimuscular soft tissue. Orbital CT should be ordered specifying fine cuts and true coronal slices.
Closed globe injury from contusion or lamellar laceration
History
The history following ocular trauma should include the details of the object that hit the eye, what the patient was doing at the time of the eye injury and what initial treatment was provided. It is very important to determine whether the object was sharp enough to lacerate the globe or the impact force was strong enough to rupture the globe (as covered in the next section of this article). This may be elicited by determining the mechanism of the injury, including the use of a sharp or blunt instrument. Lesions of the eyelids and ocular adnexa are a frequent accompanying manifestation if there was concurrent facial trauma. These are most common in the paediatric cohort and are usually caused by dog bites within the first decade of life.16,17
Examination
The examiner should first observe for the presence of lid puncture wound and oedema, proptosis, subconjunctival haemorrhages, conjunctival flap and corneo-scleral laceration. Visual acuity should be documented if the eyelids can open spontaneously. It is important not to force the swollen lid open if the mechanism of injury suggests globe laceration or rupture. RAPD and motility should also be examined to determine nerve or muscle damage. A mid-dilated pupil may indicate traumatic mydriasis. Visual field defects on confrontation testing may indicate a retinal detachment. Similarly, loss of the red reflex may also provide a clue as to whether the retina is detached or if there is a vitreous haemorrhage. Table 1 presents the red flags for ocular trauma requiring urgent referral to a tertiary centre. The next step is to systematically examine the eyelid margin, punctum of canalicular system and canthal tendons, and check for foreign bodies hidden in the conjunctival fornix. Intraocular pressure (IOP) should be assessed if the tonometer is available and when an open globe injury is determined to be unlikely. Importantly, a very low IOP may indicate an occult globe rupture. The cornea may have a partial thickness defect known as a lamellar laceration, which is best visualised with a slit lamp. Any subconjunctival haemorrhage should be noted to its furthest extent, while a conjunctival flap may indicate potential lamellar laceration to the sclera. The anterior chamber may be examined for a hyphaema. When present, the level of the hyphaema should be estimated with the patient in the upright position. Distorted pupil shape may result from dehiscence of the iris root from its base (iridodialysis). Dispersed lens matter within the anterior chamber may be seen if there is rupture of the lens capsule, and this should also be noted. Blunt trauma may lead to rupture of the lens zonules so that the lens may become subluxated or even dislocated, which is best visualised through a dilated pupil (Figure 2). If the lens is absent behind the pupil, B-scan ultrasonography (10 Hz) can be performed to look for the completely dislocated lens in the vitreous cavity if the patient is confirmed to have a closed globe injury. The retina should also be examined for signs of blunt trauma, such as choroidal rupture in the macular region and commotio retinae in the periphery (Figure 2).
| Table 1. Red flags for ocular trauma requiring urgent referral to a tertiary centre |
| History or examination findings |
Confirm or exclude |
| No or poor red reflex |
Vitreous haemorrhage, retinal detachment |
| Relative afferent pupillary defect |
Optic nerve function may be compromised by an orbital apex fracture and/or retrobulbar haemorrhage |
| Reduced vision |
Corneal infection, hyphaema, lens dislocation, vitreous haemorrhage, retinal detachment, optic nerve injury |
| Hypopyon |
Endophthalmitis |
| Peaked, abnormally shaped pupil (corectopia) pointing towards the corneoscleral wound |
Penetrating eye injury (iris prolapse)
Caution against measuring IOP in the case of a suspected penetrating injury |
| Limbal whitening and large corneal epithelial defect |
Limbal ischaemia |
| Subconjunctival haemorrhage with conjunctival flap |
Lamellar laceration or foreign body |
| Diplopia and proptosis |
Medial orbital wall or inferior orbital floor blowout fracture |
| Proptosis/increased IOP |
Retrobulbar haemorrhage
IOP – be aware of pre-existing glaucoma |
| IOP, intraocular pressure |
![Figure 2. Closed globe injury from contusion includes lens dislocation [A, B] and commotio retinae [C, D].](/getattachment/AJGP/2022/July/Eye-injuries/AJGP-07-2022-Focus-Heath-Jeffery-Eye-Injuries-Fig-2.jpg.aspx?lang=en-AU)
Figure 2. Closed globe injury from contusion includes lens dislocation [A, B] and commotio retinae [C, D].
A. Direct illumination and B. retro illumination anterior slit lamp photographs showing a lens partially dislocated superiorly because of damaged lens zonules. Surgical repair involved vitrectomy, lensectomy and sutured posterior chamber intraocular lens; C. Colour widefield retinal photograph of the left eye showing commotio retinae or a golden sheen in temporal periphery. The patient sustained a blunt force injury from his daughter, aged four years, throwing a ball at his face; D. At three months follow-up the commotio retinae had resolved spontaneously with no permanent vision loss.
Management
Patients with an RAPD, reduced vision, motility impairment and proptosis should be referred immediately to an ophthalmology service for detailed intraocular examination and orbital assessment. Patients with hyphaema, lens matter in the anterior chamber and loss of the red reflex should also be referred urgently. Microhyphaema may be managed with bed rest, Prednefrin Forte or Maxidex eye drops four times per day and a cycloplegic agent, and the IOP should be closely monitored. For injuries resulting from animal bites, prophylactic antibiotics, tetanus and rabies protocols should be followed.
Open globe injury from rupture or full-thickness laceration
History
It is essential to know the type of material that caused the eye injury. The mechanism of the injury is also important, as an intraocular foreign body (IOFB) may arise from a sharp force, leading to a penetrating or perforating eye injury, or a blunt force, leading to a globe rupture. A history of nearby metal striking metal without the use of protective goggles should raise suspicion of an IOFB. The retained material may be inert, such as glass, or retinal toxic, such as a copper fragment. It is important to note that when a metallic foreign body hits the globe, the velocity may be sufficient to enter the vitreous cavity while leaving minimal evidence of entry on the cornea or sclera. Globe ruptures occurring after a fall often have a history of prior intraocular surgery.15
Examination
When examining an eye with a suspected globe rupture, it is important not to place any pressure on the globe. A fluorescein assessment under blue light should be done to exclude a positive Seidel test. Signs of an open or penetrating globe injury include: a penetrating lid injury, shallow anterior chamber, hyphaemia, peaked pupil, lens dislocation and vitreous haemorrhage. A hypopyon indicates severe infection within the eye, and an IOFB must be suspected. A subconjunctival haemorrhage alone may occur after closed globe trauma, and it can be managed conservatively. However, occasionally it can be a sign of a ruptured globe when associated with IOP and very deep anterior chambers. A vitreous haemorrhage is another sign of serious intraocular trauma. This may be noted with a direct ophthalmoscope when the examiner observes loss of the red reflex when compared with the other eye. All patients presenting with a vitreous haemorrhage should be referred for further examination to exclude a globe rupture and/or retinal detachment. If the globe is obviously open (eg iris prolapse through the cornea or uveal prolapse through a defect in the sclera), IOP and motility should not be checked. If there is significant eyelid swelling precluding direct inspection of the globe and the suspicion of open globe injury is high based on history, manipulation of the eyelids should be deferred until after radiological investigation of the orbit as there are classic CT signs that can be used to diagnose globe rupture (Figure 3). In any patient presenting with ocular trauma, additional injuries such as neck trauma (carotid artery dissection) and/or facial or skull fractures should be excluded.
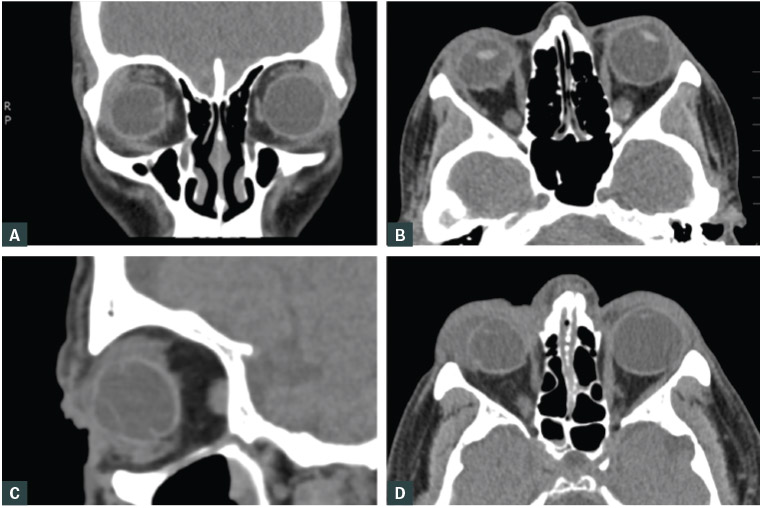
Figure 3. Open globe injury diagnosed on radiological signs
A. Coronal and B. transverse computed tomography (CT) scans of the orbits showing a collapsed right globe with distorted contour when compared with the rounded left globe due to a right anterior scleral laceration from glass fragments. In addition to the scleral wound repair, the patient required a vitrectomy to repair an anterior retinal tear; C. Sagittal and D. transverse CT scans of the right orbit showing a distorted contour consistent with a ruptured globe. The patient required multiple retinal detachment surgeries after primary repair of the scleral wound.
Management
Any open globe injury requires an immediate referral to an ophthalmology service, and oral ciprofloxacin 750 mg twice daily should be prescribed on route. Intravenous antiemetics may be considered for patients with nausea and vomiting in order to reduce IOP. A globe ruptured by blunt trauma should be managed in the same way as a globe laceration. An eye shield should be placed over the injured eye for protection while the patient is transferred to a tertiary referral centre. The use of eye pads should be avoided to prevent any pressure on the globe. Ointments should also be avoided in the case of an open globe. The location and presence of an IOFB may be determined with a plain film X-ray of the head and/or CT scan of the orbits with fine cuts (1–2 mm) if not obvious on clinical examination (Figures 3 and 4). The entry wound for small or sharp foreign bodies may be so small as to self-seal, and therefore diagnosis of IOFB may depend on radiology. A magnetic resonance imaging scan is generally unnecessary and is contraindicated in those with metallic foreign bodies. Prophylaxis for tetanus infection is required for a patient with conjunctival, scleral and/or periocular lacerations as well as IOFBs. Adequate analgesia and antiemetics should also be considered.
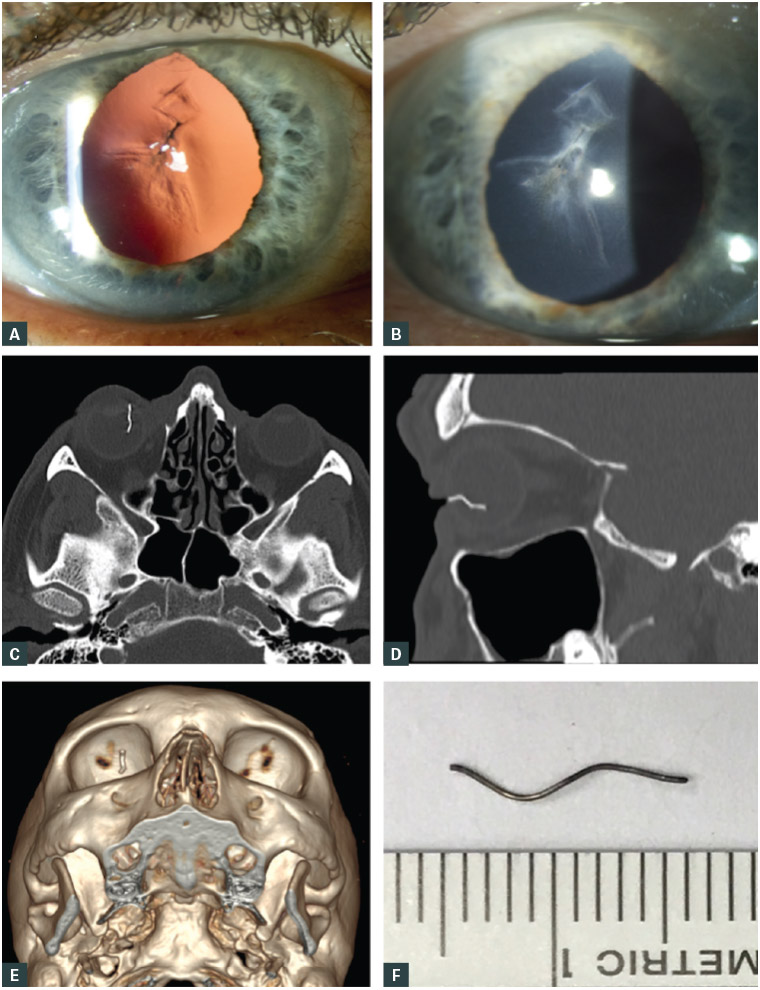
Figure 4. Penetrating intraocular injuries diagnosed on clinical and radiological signs
A. Retro illumination and B. direct illumination anterior slit lamp photographs of a central corneal scar due to a penetrating eye injury requiring immediate removal of the ruptured lens and suturing of the corneal wound; C. Transverse and D. sagittal computed tomography (CT) scans showing a metallic intraocular foreign body in the right eye of a patient who initially presented to his general practitioner for treatment of a suspected foreign body. The patient was treated with chloramphenicol ointment, and the eye was patched for three days. He was later referred to the emergency department with suspected endophthalmitis. Following a CT scan that confirmed an intraocular metallic foreign body, the patient underwent an urgent vitrectomy, removal of the metallic foreign body and received intravitreal antibiotics; E. The linear foreign body can be seen on three-dimensional reconstruction, but the scleral entry wound had sealed completely by the time of surgery; F. A hole in the sclera was created to remove the 10 mm wire.
Conclusion
There are many possible causes of ocular trauma. The clinician must determine whether a patient with ocular trauma can be reassured or, instead, requires urgent referral to the local emergency department for further investigation. If any uncertainty exists, onward referral is appropriate granted the potential for serious underlying sight- and eye-threatening pathology, such as missed IOFBs.