Stable and pain-free thumb function and pinch is vital for personal care, work, domestic and leisure activities. Thumbs are used for fine motor tasks such as writing and texting on mobile telephones. Power pinch is needed to grip a hammer and open a jar. When a painful thumb gets worse instead of better, a patient frequently presents to their general practitioner (GP). Clear management pathways prevent repeat presentations. This article covers three thumb conditions: acute trauma (ulnar collateral ligament [UCL]), repetitive trauma (De Quervain’s tendinopathy) and chronic progression (basal thumb osteoarthritis). For each condition, recommendations are made regarding taking a history, clinical assessment, early intervention and referral for imaging, hand therapy and/or non-GP specialist intervention.
Ulnar collateral ligament injury of the thumb
Injury to the UCL at the metacarpophalangeal (MCP) joint is very common. The ligament is injured by valgus/abduction forces to the thumb, such as being hit by a ball or falling onto the thumb, especially when holding a tennis racquet or the stock when skiing. Patients with ligament strains will report pain and difficulties with pinch grip activities such as turning a key and squeezing a peg.
The UCL comprises both proper and accessory fibres and is approximately 4–8 mm in width and 12–14 mm in length. The proper collateral ligament is most stable in 30° MCP joint flexion, while the accessory ligament is most taut in full MCP joint extension.1 Distal tears comprise 90% of all presentations, with 50% of all UCL injuries having an associated avulsion fracture. A Stener lesion is a complete tear of the ligament with interposition of the adductor aponeurosis between the avulsed ligament/bone fragment and its insertion point. The avulsed ligament stump cannot reattach itself because the adductor aponeurosis blocks the insertion point, and surgical intervention is required.1–3
The clinical integrity of the ligament needs to be tested in both full extension and 30° flexion (Table 1). Plain X-ray and ultrasonography imaging can be informative. To confirm a Stener lesion, magnetic resonance imaging has greater sensitivity and specificity (100%) when compared with ultrasonography, which has 88% sensitivity and 83% specificity.2,3
| Table 1. Referral pathways for ulnar collateral ligament injury of the thumb |
| History |
Clinical testing |
GP early intervention |
GP-referred imaging |
Refer to hand therapy |
Refer to non-GP specialist |
Abduction force +/– pain and subluxation
Tender at MCP joint within thumb web
Mild instantaneous pain on pinch |
Grade 1 ligament strain
Tender to palpation of MCP within thumb web.
Test by stabilising the metacarpal neck and provide a radially directed force to the proximal phalanx with MCP joint in extension. Repeat in 30° flexion. May or may not have mild laxity and end-range pain when compared with the unaffected thumb. |
Education: splint will be needed for one month. Patients can still use hand and move wrist in splint. Sprains heal without surgery. |
X-ray (PA, oblique, lateral)
Ultrasonography for MCP collateral ligaments
|
✓ |
|
Dislocation requiring reduction
Tender at MCP joint within thumb web
Moderate instantaneous pain on pinch
Mild resting ache |
Grade 2 partial ligament tear
Tender to palpation of MCP joint within thumb web.
Test as described for Grade 1 ligament strain.
Moderate laxity and end-range pain when compared with the unaffected thumb. |
Education: ligaments are slow to heal, splinting will be needed full time for six weeks. Patients still use hand and move wrist in splint. Partial ligament tears heal without surgery, and total hand therapy is approximately 12 weeks. |
X-ray (PA, oblique, lateral)
Ultrasonography for MCP collateral ligaments
|
✓ |
|
Dislocation requiring reduction
Unable to load thumb in pinching activities as a result of sense of thumb collapse rather than pain
Vague ache at the MCP joint |
Grade 3 complete ligament tear
Test as described for Grade 1 ligament strain.
Greater than 30° angulation; increased laxity of 15° when compared with the uninjured thumb and lack of end feel. No pain to end range (except in very acute phase). |
Education: if the adductor aponeurosis is interposed, the ligament needs surgery. The timing of surgery is non-critical and can be planned to suit the patient. The thumb will be in a splint for 4–6 weeks after surgery, and total post-operative hand therapy takes approximately
12 weeks. |
X-ray to check for avulsed fragment (Stener lesion)
Refer to non-GP specialist for MRI |
✓ |
✓
Surgeon |
No improvement in symptoms despite splinting
Pain +/– instability on attempted splint weaning |
Treatment resistant for >3 months
Grade 2–3: Differential diagnosis of pain from prolonged splinting versus instability/Stener lesion |
Education: ligaments are very good at communicating and are designed to broadcast pain; therefore, instability is the critical measure of ligament healing, not pain. |
Refer to non-GP specialist for MRI
|
✓
When ligament tests are stable, refer to hand therapy for supervised orthotic weaning and graduated exercise |
✓
Surgeon (when ligament tests are unstable) |
| GP, general practitioner; MCP, metacarpophalangeal; MRI, magnetic resonance imaging; PA, posterior-anterior |
Current concepts in management
Static custom orthoses achieve good results in 85–91% patients.4 Stiffness is a common complication. Use of a hinged orthosis permitting limited range of motion of the MCP in the flexion/extension plane has been reported to be comfortable and allow greater function. Hand therapists have the skills to fabricate these.4
In animals, stress to collateral ligaments provides a greater ratio of mature to immature cross-linked collagen, enhancing healing and stability. Hand therapists are trained in how and when to apply controlled stress to ligaments.2,4
Hand therapy for UCL injury
The first line of hand therapy treatment is a hand-based opponens orthosis, which can be custom made by hand therapists (Figure 1A). A radially based orthosis protects the UCL up to 100 N force, considering maximum load to failure is 84 N.5
Short arc early motion protocols may be implemented under the supervision of a hand therapist.
Splinting is continued full time for 4–6 weeks, followed by mobilisation and strengthening at 6–8 weeks post injury.
Regarding sport, hand therapists can fabricate minimal splints to be taped on for return to play.
Weaning of orthoses is often slow as the thumb is an integral part of function and easily aggravated. Readiness for orthotic weaning is determined via joint stability rather than pain.
Early identification of Stener lesions is critical because they will not heal conservatively and require surgical intervention (Table 1).

Figure 1. Custom orthoses fabricated by hand therapists
A. Hand-based opponens orthosis for either ulnar collateral ligament injury or basal thumb osteoarthritis; B. Orthosis suitable for De Quervain’s tendinopathy
Photographs used with permission from the Australian Hand Therapy Association
De Quervain’s tendinopathy of the thumb (stenosing tendinopathy)
De Quervain’s tendinopathy generally affects postpartum women and adults over 40 years of age. Readers are directed to a recent article in Australian Journal of General Practice (AJGP) for further information.6 In De Quervain’s tendinopathy, two thumb tendons – abductor pollicis longus (APL) and extensor pollicis brevis (EPB) – are prevented from gliding. Tethered by the extensor retinaculum, APL and EPB pass through an osseofibrous tunnel near the wrist. In response to excessive compression and shear forces, the tunnel narrows (stenosis). Type 1 tendinopathy is stenosis of both APL and EPB; type 2 is EPB only.7,8 Research over the past 20 years9,10 indicates the pathophysiology may be myxoid degeneration and mucopolysaccharide accumulation – in effect, the body detects friction and responds with fibrosis. Therefore, prolonged, repetitive, forceful wrist deviation/flexion in combination with loaded pinching can bring about De Quervain’s tendinopathy, as can direct impact trauma.11 Clinical tests for De Quervain’s tendinopathy have low specificity. The wrist hyperflexion abduction of thumb (WHAT) test has greater sensitivity and specificity than the Finkelstein test and Eichoff’s test, which are aggressively provocative.12 A novel variation is the ‘selfie test’, using a mobile telephone with the thumb on the camera button.13
Current concepts in management
De Quervain’s tendinopathy causes suffering. One study found that people with De Quervain’s tendinopathy scored higher on a self-rated survey of disability than people with thumb amputation.14
Steroid injections may be effective in alleviating pain in De Quervain’s tendinopathy, particularly in combination with orthoses.15 In one double-blind randomised controlled trial, researchers compared injecting a corticosteroid with injecting a nonsteroidal anti-inflammatory drug (NSAID). Finding the corticosteroid significantly superior, they postulated the mechanism of action may be something other than anti-inflammatory.16 Research over the past 20 years has indicated that De Quervain’s tendinopathy pain is mechanical rather than inflammatory.7,8,17 If research shows De Quervain’s tendinopathy is mechanical and non-responsive to NSAIDs, there is pause for thought in traditional approaches. In a science-driven paradigm shift, DeQuervain’s tendinopathy is no longer considered an inflammatory condition. Best practice hand therapy builds muscular stability to sustainably reduce the mechanical stress on APL and EPB tendons and ensure functional wrist proprioception.
Hand therapy for De Quervain’s tendinopathy
Hand therapists fabricate wrist/thumb orthotics. Ideally orthoses will be rigid, preventing wrist deviation and proximal thumb motion (Figure 1B). Postpartum women often struggle to wear orthoses full time, tending to remove them for the tasks during which they are most needed. Dilution of the orthotic-wearing regimen requires a longer period of splinting, within reason. Prolonged immobilisation is harmful, and if splinting exceeds three months, surgery should be considered (Table 2).
| Table 2. Referral pathways for De Quervain’s tendinopathy |
| History |
Clinical testing |
GP early intervention |
GP-referred imaging |
Refer to hand therapy |
Refer to non-GP specialist |
Postnatal
Sharp radial wrist pain when feeding, bathing and positioning baby in restraints |
WHAT or ‘selfie test’ for type 1
Resisted thumb extension (hitchhiker sign) for type 2 |
Education: wrist flexion and deviation and thumb pinch are aggravators, consider baby handling ergonomics |
Case-by-case referral for ultrasound-guided corticosteroid injection |
✓ |
|
Acute
Sharp radial wrist pain
Report of change in task demands or task ergonomics, such as change of work role, covering during a period of short staffing, repetitious forceful motions (eg hand-wringing laundry) |
WHAT or ‘selfie test’ for type 1
Resisted thumb extension (hitchhiker sign) for type 2 |
May need suitable duties and graduated return to work |
Ultrasound-guided corticosteroid injection |
✓ |
|
Chronic
Insidious onset of sharp radial side wrist pain, intermittent then reproducible |
WHAT or ‘selfie test’ for type 1
Resisted thumb extension (hitchhiker sign) for type 2 |
May need suitable duties and graduated return to work |
Ultrasonography to check for anatomical anomalies such as multiple tendon slips of APL and EPB |
✓ |
✓
Surgeon |
Treatment resistant
May have yellow flags for persistent pain, including report of forearm pain |
Disabilities of Hand, Shoulder and Arm survey score over 50%
WHAT or ‘selfie test’ for type 1
Resisted thumb extension (hitchhiker sign) for type 2 |
May need a worksite assessment |
Ultrasonography to check for anatomical anomalies, such as multiple tendon slips of APL and EPB |
✓
For pain management |
✓
Surgeon or pain specialist |
| Traumatic impact to radial wrist followed by reproducible radial side wrist pain |
WHAT or ‘selfie test’ for type 1
Resisted thumb extension (hitchhiker sign) for type 2 |
May need suitable duties and graduated return to work |
Referral to non-GP specialist for MRI |
✓
For symptom management to function pending specialist assessment |
✓
Surgeon |
| APL, abductor pollicis longus; EPB, extensor pollicis brevis; GP, general practitioner; MRI, magnetic resonance imaging; WHAT, wrist hyperflexion abduction of thumb |
Dynamic stabilising exercises commence immediately. The wrist and thumb tendons learn to activate and, when splinting is complete, are prepared for force and load. Mid-phase rehabilitation focuses on tendon gliding between APL and EPB. Resilience is further enhanced by eccentric loading after splint weaning.17,18
Ergonomic advice starts day 1 (Figure 2) to address root causes.

Figure 2. Ergonomics of baby care for people with De Quervain’s tendinopathy. The mother pictured developed De Quervain’s tendinopathy in her non-dominant right wrist.
A. She tries to avoid thumb pinch and wrist deviation, yet because of De Quervain’s tendinopathy she cannot tolerate wrist flexion for very long; B. She uses her leg to keep the baby safe and stable while resting her right wrist. When the baby was younger, she used the same leg posture to feed the baby using her elbow and keeping her wrist and thumb neutral.
Photographs used with permission from Vicki Strelan/the Australian Hand Therapy Association
Measurable improvement is typically observed week by week of full-time wear in a one-month splinting program.
Traumatic De Quervain’s tendinopathy can be resistant to conservative intervention, thus immediate referral for surgical opinion is recommended. Examples of traumatic De Quervain’s tendinopathy could include the mechanic whose wrist was crushed when the jack fell sideways, or the kitchenhand who stood up quickly, impacting the radial wrist on the underside of the steel bench (Table 2).
Basal thumb osteoarthritis
Osteoarthritis at the base of the thumb is the most common type of arthritis, affecting the non-dominant hand first because of the biomechanics of power pinch.19–21 Readers are directed to a recent article in AJGP for further information.19
Thumb osteoarthritis is progressive:
- Wear and tear results in attenuation of the basal thumb ligaments, particularly the oblique ligaments and the dorsal radial ligament.22
- The first metacarpal becomes unstable and slides from the saddle of the trapezium, causing a ‘step deformity’. In early osteoarthritis this is a dynamic subluxation, and as progression along the disease spectrum occurs, in advanced osteoarthritis the joint space is obliterated and fused in a permanent step deformity (Figure 3A).
- The long thumb tendons dominate, causing the MCP to collapse into too much extension or too much flexion. The adductor pollicis muscle contracts and tightens the webspace.
- Muscle weakness leads to an abnormal imbalance of forces across the joint. This results in further instability, pain and altered reflex patterns.
Classification by Eaton-Littler covers four stages of basal thumb osteoarthritis. Stage 1 is mild base-of-thumb instability. Stage 2 is a loss of joint space with development of osteophytes.19 Stage 3 includes sclerosis and osteophytes >2 mm, and Stage 4 adds wrist degeneration.23
Current concepts in management
X-ray findings do not necessarily correlate with pain and disability.23,24
Loading the thumb with first dorsal interrosseus muscle activation decreases vertical displacement of the first metacarpal and protectively maintains joint space.25
Obesity is a risk factor. Adipokines have pro-inflammatory properties and can initiate and progress osteoarthritis.26,27
Hand therapists recognise the highly proprioceptive nature of the basal thumb joint.22,28
Hand therapy for basal thumb osteoarthritis
Hand therapy improves function for patients with all stages of basal thumb osteoarthritis, and hand therapists can provide appropriate rehabilitation following surgical arthroplasty or joint fusion (Table 3).
| Table 3. Referral pathways for basal thumb osteoarthritis |
| History |
Clinical testing |
GP early intervention |
GP-referred imaging |
Refer to hand therapy |
Refer to non-GP specialist |
Basal thumb pain (low-grade frequent ache, sharp instant pain on strong pinch) +/– crepitus
Typically non-dominant thumb presents first |
Eaton-Littler Stage 1–2
Will be tender to palpation at thumb CMC joint
Mild step deformity, reducible with gentle traction of first metacarpal; patients report this action as relieving
Palpable CMC subluxation on key pinch |
Education:
- Osteoarthritis is ‘wear and tear’ arthritis, not systemic, and it starts with ligament attenuation
- Identify occupational risks
- Early intervention can arrest progression
- Balance activity and rest
- Consider nutrition
- Consider aids for daily living
|
X-ray: PA hand/wrist; lateral in pinch position |
✓ |
|
Thumb MCP pain +/– basal thumb pain (low-grade constant ache, sharp instant pain on strong pinch) +/– crepitus, tendency for thumb MCP to collapse into hyperflexion or hyperextension, reduced fine motor coordination
Non-dominant thumb is more commonly affected than dominant thumb
Limitations to activities of daily living with tasks such as meal preparation, lifting a kettle and managing buttons on clothing |
Eaton-Littler Stage 2–3
May be tender to palpation at thumb CMC joint and MCP joint
Obvious step deformity that may be resistant to traction of the first metacarpal or may be non-reducible
May have thumb web shortening
May have unstable MCP where the head of the metacarpal collapses volarly and the phalanges hyperextend |
- Osteoarthritis is ‘wear and tear’ arthritis, not systemic, and it starts with ligament attenuation
- Balance activity and rest
- Consider nutrition
- Consider aids for daily living
|
X-ray: PA hand/wrist; lateral in pinch position |
✓ |
✓
Surgeon |
Radial wrist pain; constant ache; aggravated by activities involving impact, repetition and moderate manual handling; will have inflammatory aggravations, including night waking from pain
Severe range-of-motion limitations |
Eaton-Littler Stage 4
Thumb deformities as for Eaton-Littler Stage 2–3 |
- May need permanent work restrictions
- Balance activity and rest
- Consider nutrition
- Consider aids for daily living
|
X-ray: PA hand/wrist; lateral in pinch position |
✓ |
Case by case
Surgeon
Rheumatologist
Pain specialist |
| CMC, carpometacarpal; GP, general practitioner; MCP, metacarpophalangeal; MRI, magnetic resonance imaging; PA, posterior-anterior |
Overall, orthotics are tolerated well as they decrease pain and improve function.
In prescribing orthoses, hand therapists perform activity analysis and collaborate closely with their patients. Various designs are available, both prefabricated and custom made (Figure 1A). No design is superior to others. The best orthosis is one that is comfortable, relieves symptoms and may be worn for rest and activity.
Joint protection techniques decrease forces across the basal thumb joint, minimising aggravation and slowing progression. Mainstays include aids to daily living, pacing activity with rest and using large muscles to protect weak joints.
Exercises are important to improve stability and correct imbalanced forces.29 Hand therapists are trained to understand which muscles deform and which muscles stabilise (Figure 3B and 3C).
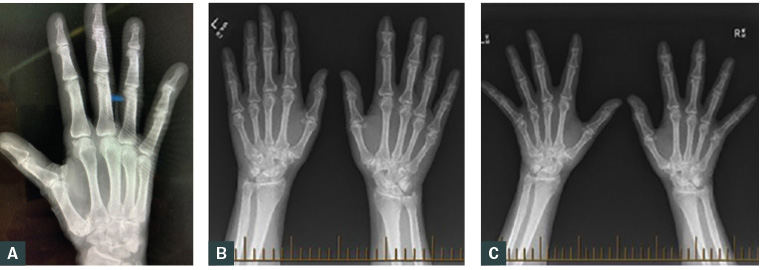
Figure 3. Radiographs of two patients with basal thumb osteoarthritis
A. A patient with Eaton-Littler Stage 3 osteoarthritis, with fused step deformity and metacarpophalangeal collapsed into hyperextension; B. A patient with Eaton-Littler Stage 2 osteoarthritis. The patient commenced regular stabilising exercises and orthoses; C. Five years later, the thumb osteoarthritis of the patient shown in Figure 3B had not progressed and remained classified Stage 2.
Figure 3A used with permission from Rebecca Crowley/the Australian Hand Therapy Association
Figures 3B and 3C used with permission from Vicki Strelan/the Australian Hand Therapy Association
Conclusion
A collaborative approach between GPs and hand therapists benefits patients with common thumb conditions. It is incumbent on Accredited Hand Therapists (as awarded by the Australian Hand Therapy Association [AHTA]) to stay abreast of current evidence and apply clinical reasoning in upper limb treatment from neck to fingertips. Knowledge of referral pathways can reduce the number of presentations to GPs for the same condition and ensure early intervention for patients with painful thumbs.
Key points
- Pain near the thumb web may be related to instability from injury to the UCL. The critical indicator is stability rather than pain. It is important to test the joint in both extension and flexion.
- It is important to keep a high index of suspicion for Stener lesions, which require surgical intervention, not hand therapy.
- De Quervain’s tendinopathy should be managed as a fibrosis rather than an inflammatory condition.
- Basal thumb arthritis begins with ligament instability and frequently affects the non-dominant thumb first; orthoses and stabilising exercises can modify the progression.