Case
A boy aged one year and seven months was brought by his mother to the general practice clinic with a three-month history of recurrent wheezing, especially when active. There were no symptoms of cough, fever, difficulty breathing or choking. There was no personal or family history of asthma, allergy or eczema. On further questioning, the boy’s mother was able to recall the first episode of wheezing at a birthday party.
On examination, the child was active and not tachypneic. His vital signs were normal, and there was no stridor or audible wheezing. Lung auscultation revealed intermittent wheeze with equal breath sounds. Other examination findings were not significant.
Question 1
What are the causes of recurrent wheezing in the preschool age group?
Question 2
What is the most appropriate investigation at this stage?
Question 3
What are the radiographic features seen in Figure 1?
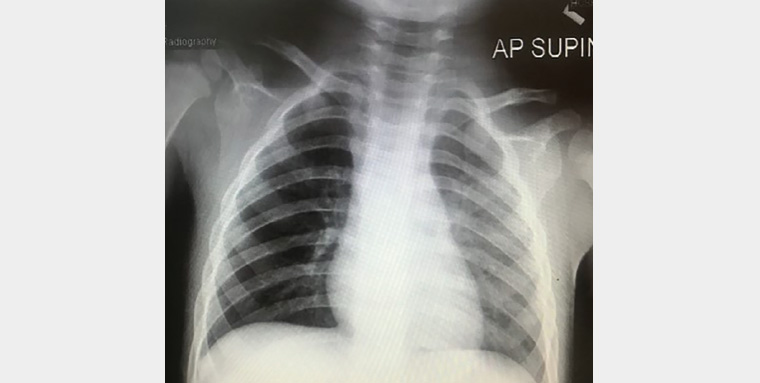
Figure 1. Chest X-ray of patient
Question 4
Combining the clinical and radiographic findings, what is the most likely diagnosis?
Question 5
How would you further manage this patient?
Answer 1
Recurrent wheezing has been estimated to occur in one-third of children of preschool age.1 The most common cause is recurrent viral-induced wheeze. Bronchiolitis and viral pneumonitis are more likely if the patient has coryzal symptoms.2 However, management of recurrent viral-induced wheeze is similar to that of bronchiolitis and viral pneumonitis, and the distinction between these conditions is sometimes arbitrary.2
The next most common cause of wheezing is asthma, which affects 15–20% of the paediatric population.2 Children usually present in early childhood with gradual onset of daily wheeze that improves with a trial of salbutamol.2 The presence of atopy is associated with persistent asthma.3
An important cause that must be ruled out is foreign body aspiration (FBA). In the case of an acute presentation, a clear history of choking followed by cough and rapid breathing can usually be obtained. When presentation is delayed, children usually present with an acute onset of non-specific respiratory symptoms.2
Answer 2
Children with recurrent wheezing should be investigated with a chest X-ray (CXR; Figure 1).1 This can identify congenital anomalies of the lung, parenchymal lung disease, possible foreign body and cardiac abnormalities.4
Answer 3
There is presence of right lung hyperlucency with no mediastinal shift, atelectasis or foreign body seen.
Answer 4
In a child with non-specific respiratory symptoms with unilateral lung hyperlucency on CXR, FBA is the most likely diagnosis. Most foreign bodies are radiolucent and not visualised on CXR. However, the presence of unilateral hyperlucent lung and post-obstructive lobar or segmental infiltrates should raise suspicion of FBA.5 It is important to note that CXR may be normal in approximately 50% of FBA cases and should not be used to exclude the diagnosis.5
Answer 5
FBA is a medical emergency. The next management step is to proceed with appropriate hospital referral, preferably to a centre with an experienced paediatrician; ear, nose and throat surgeon; and anesthetist for diagnostic and therapeutic bronchoscopy. In cases lacking suggestive findings, diagnosis can also be accomplished with high-resolution computed tomography (HRCT) of the thorax.5 HRCT has the advantage of avoiding unnecessary invasive intervention if the finding is normal.5 Additionally, HRCT can locate the exact site of foreign body, making retrieval easier.
Case continued
The child was referred to a tertiary hospital for further management. HRCT of the thorax showed an irregular lesion at the distal right main bronchus causing luminal obstruction (Figure 2). The patient underwent bronchoscopy under general anaesthesia, and a small plastic flower decoration was removed from the right main bronchus (Figure 3). Bronchial lavage culture grew Klebsiella pneumoniae. The patient was discharged after completing one week of antibiotics.
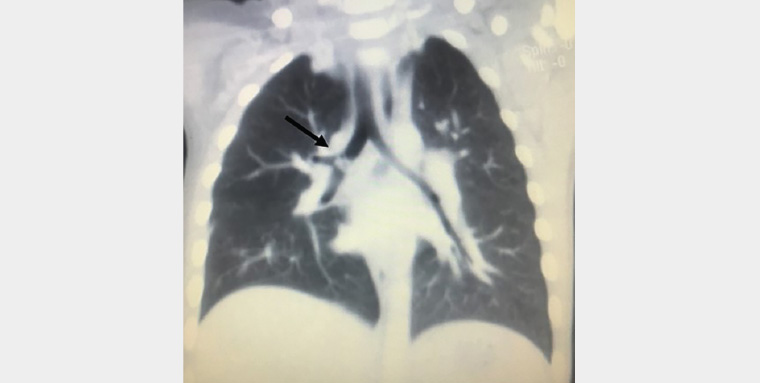
Figure 2. High-resolution computed tomography of the thorax showing an irregular lesion at the distal right main bronchus (arrow)
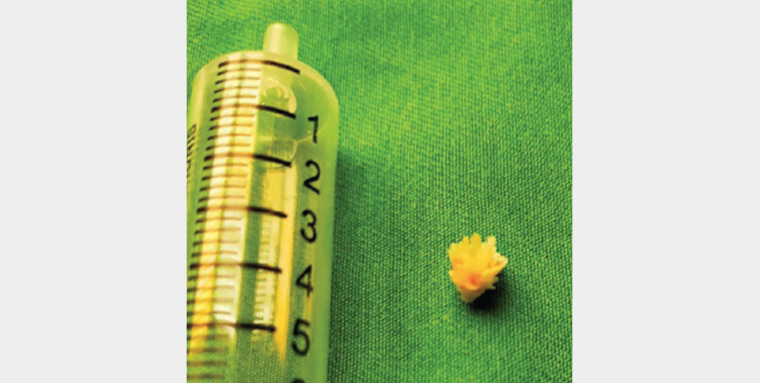
Figure 3. A plastic flower decoration removed from the right main bronchus
Question 6
Why are children at higher risk of aspiration than adults?
Question 7
How common is delayed presentation of FBA?
Question 8
What public health measures must be taken to prevent FBA?
Answer 6
Children are more likely to aspirate than adults because of their lack of molar teeth, immature swallowing mechanism and weak protective laryngeal reflexes.6 In addition, they like to explore unfamiliar items using their mouths and have a tendency to play while eating.7 The incidence of FBA is highest in children aged between one and three years, and most studies have shown male predominance.8
Answer 7
In approximately two-thirds of cases, patients present immediately to the emergency department, while the remainder usually present to general practice.7 This is because approximately half of FBA cases occur without adult supervision, hence the choking event is not observed.9
Answer 8
FBA is the leading cause of accidental death in children.10 In primary care settings, it is important to increase awareness among parents and carers. Emphasis should be placed on preventive measures such as delaying solid food until the child can swallow effectively, close adult supervision during eating and playing, and keeping ‘high-risk’ objects out of reach. All new parents and carers should be familiar with basic resuscitation techniques and manoeuvres to perform in the event of an acute episode of choking.9 These manoeuvres include back slaps in children with ineffective cough followed by abdominal thrusts if back slaps are ineffective.11
Educational campaigns can also be conducted at nurseries and schools.
Key points
- FBA must be considered in children with non-resolving respiratory symptoms.
- Chest radiography is indicated for children with recurrent wheezing.
- Primary care physicians can increase awareness among parents during clinic visits.