The COVID-19 pandemic has highlighted the relevance of international travel for public health. There have been major changes in the speed and extent of the spread of pandemics over the course of human history. In medieval times, bubonic plague moved across Europe at human walking speed, whereas by 1918 H1N1 influenza A virus was able to spread via shipping routes to most parts of the world. The advent of international air travel changed the situation dramatically, with infections such as influenza, dengue, Zika and coronaviruses able to move around the world in a matter of days or even hours.
The risk of disruption to international travel has also been made evident by the COVID-19 pandemic. The impact of the pandemic on international arrivals into and departures from Australia is shown in Figure 1. Many Australians living overseas were not able to return to Australia, and international tourist travel and travel to visit friends and relatives collapsed at the onset of the pandemic in February 2020. However, as shown in Figure 1, international travel is starting to recover (February 2022) as restrictions are eased and airlines re-establish services.
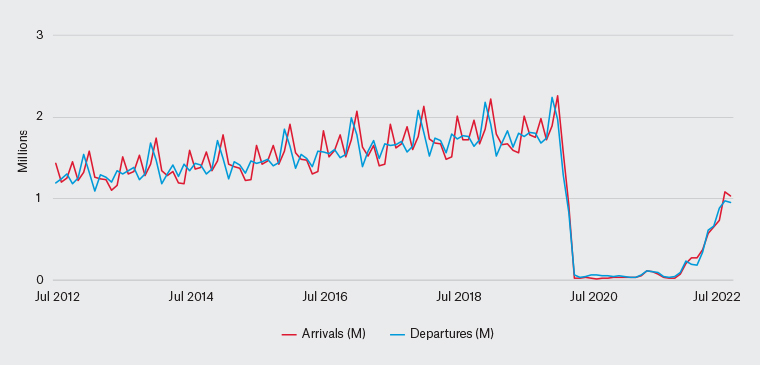
Figure 1. Total overseas arrivals and departures, June 2012 to July 2022. Source: Australian Bureau of Statistics. Overseas Arrivals and Departures. Released 13 September 2022.30
Note: Provisional data for the most recent month has not had the full quality assurance methods applied as done for the earlier months.
M, millions
COVID-19 and travel
In this new era, travellers and their health advisors are faced with weighing up the risk of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) while overseas, including the emergence of new variants. Being unvaccinated, increasing age and underlying health conditions are risks for developing a serious infection that could be fatal. The recently released Australasian College of Tropical Medicine travel health guidelines provide an approach to risk assessment and giving advice.1
The Australian Government Smartraveller website provides a step-by-step planning guide for travel during the COVID-19 pandemic. This includes making sure that people have downloaded a copy of their international COVID-19 vaccination certificate. Although not mentioned on the Smartraveller website, taking a printed copy of the certificate when travelling, in addition to a digital version, is a good precaution. The website strongly discourages international travel by unvaccinated Australians because of the health risks. When leaving the country, travellers may be asked to provide proof of COVID-19 vaccination status, but, from 18 April 2022, travellers no longer need an exemption to leave Australia if they do not meet the definition of fully vaccinated.
A related challenge is understanding and complying with the varied and changing vaccination, testing and quarantine requirements across destination countries. A useful online resource for up-to-date information is the US State Department website. That website maintains a comprehensive listing, including a summary of the COVID-19 situation, COVID-19 testing availability and entry and exit requirements by country.2 The information is written from the perspective of US travellers, but most of the information would be relevant to Australians.
Flight delays, cancellations and lost luggage are much more common as airports, airlines and other travel services struggle with re-establishing staffing and services, and continue to experience workforce disruptions due to COVID-19 and other respiratory illnesses. It is therefore more important than ever that people with long-term conditions, such as diabetes, make sure they carry medication in their hand luggage and plan ahead for possible disruption.3
Some people are concerned and will ask for information about the risk of SARS-CoV-2 transmission on aircraft. This is not an easy question to answer because there are a limited number of good-quality studies on flight-associated SARS-CoV-2 transmission.
4 There have been documented instances of transmission, included a published report from a five-hour flight from Sydney to Perth that had passengers on board from the Ruby Princess cruise ship.
5 A review of air travel and COVID-19 found evidence that the risk of transmission is reduced by passengers and crew wearing masks and by hygiene precautions, including social distancing before boarding.
6 During flight, mask wearing should continue, with minimal unmasked time when eating and drinking. Hand sanitising and disinfection of high-touch surfaces may also help reduce the risk of transmission inflight.
Emergence or resurgence of other infectious disease hazards
The disruption of health services and immunisation systems since the onset of the COVID-19 pandemic has seen the resurgence of a number of infectious diseases.
Measles
The most notable resurging disease is measles. According to United Nations Children’s Fund (UNICEF) and the World Health Organization (WHO), worldwide cases of measles increased by 79% in the first two months of 2022 compared with the same period in 2021.
7 The largest numbers of cases were in Africa and the Eastern Mediterranean region. The WHO estimated that, in 2020, 23 million children missed out on basic childhood vaccines through routine health services, the highest number since 2009.
7 This resurgence emphasises the importance of Australian travellers born after 1966 being sure they have two documented doses of the MMR (measles, mumps, rubella) vaccine.
Influenza
The situation with influenza is another concern, with waning levels of population immunity given the low transmission of influenza during the COVID-19 pandemic, but the risk of resurgence with the resumption of international travel. Although Australia recorded zero deaths from influenza in 2021, and only one hospitalisation, this changed markedly in 2022 with a surge of cases; government immunisation authorities have been reminding people of the importance of annual vaccination. This advice is particularly relevant for travellers.
Antimicrobial resistance
While attention has been focused on COVID-19, the global problem of antimicrobial resistance (AMR) continues to develop. Indeed, there is some evidence that the COVID-19 pandemic is accelerating the problem of AMR.8 This includes evidence that the shift to telemedicine is associated with increased antibiotic prescribing.9 Antibiotic monitoring by the US Centers for Disease Control and Prevention (CDC) showed an increase in antibiotic use as clinicians face uncertainty as to whether a respiratory infection is due to SARS-CoV-2 or another cause.10 A review of data from COVID-19 cases, mostly in Asia, found that more than 70% of patients received antimicrobial treatment.11 Given that the increased use of antibiotics is associated with increased resistance, all these factors favour the emergence of AMR.
Travel, including for healthcare reasons, has been a factor in the spread of AMR because travellers can become colonised by pathogens with resistant genes.12 One such example is colonisation of the gut by extended-spectrum β-lactamase-resistant Enterobacteriaceae. These bacteria carry a gene that confers resistance to all beta-lactam antibiotics and has been found to confer resistance to fluoroquinolones and aminoglycosides. To make matters worse, the resistance is highly transferable among Enterobacteriaceae, including to Escherichia coli.13
Japanese encephalitis
Unrelated to the pandemic, climate and other environmental changes are altering disease risk. The most high-profile local example is the emergence of Japanese encephalitis virus (JEV) in Australia. This is likely to be related to climate change and increased mosquito activity during the La Niña event of 2021–22. JEV has been detected intermittently over December and January in the Torres Strait since 1995, but its occurrence in south-eastern Australia since February 2022 is a new phenomenon.
Dengue
While JEV has been in the news, dengue virus has been increasing globally, with the disease now endemic in more than 100 countries in the WHO regions of Africa, the Americas, the Eastern Mediterranean, South-East Asia and the Western Pacific.14 Climate change may again be a factor in increased dengue transmission, with warmer temperatures favouring the primary mosquito vector Aedes aegypti. In addition, the secondary vector, Aedes albopictus, is being spread via the international trade in used tyres. Urbanisation is also a factor in providing breeding sites for mosquitoes that transmit dengue.
Monkeypox
Previously confined to Africa, monkeypox has now spread globally. The increase in cases is likely to be related to cessation of smallpox vaccination programs in the 1980s. Human-to-human transmission can result from close contact with the skin lesions of an infected person, recently contaminated objects (eg towels) or, less commonly, via respiratory secretions. Although monkeypox is not specifically a sexually transmissible disease, men who have sex with men are a high-risk group for infection.15
New models of travel in the pandemic age
An important driver for the recovery in international travel is the wish to reconnect with friends and family living overseas. In this case, travellers may be willing to put up with the complexities, uncertainties and the relatively high cost of airfares, whereas the leisure market is likely to be slower to recover and business travellers are making more use of technology. Travel health insurance is more important than ever as a safety net for travellers, and careful attention to what is covered is needed because many policies have exclusions for COVID-19-related travel disruption. Travellers may need to seek out and potentially pay more for insurance, and have a contingency plan in case travel is disrupted by COVID-19.
The experience of the pandemic has led some destinations to reconsider their tourism model. Some destinations do not want to return to previous approaches to mass tourism, which have put strains on infrastructure, the environment and the amenity of the local population. The return of Australian travellers to Bali will be welcomed by the tourism and hospitality sectors, but the government is seeking to develop a new tourism model that better protects the environment and distributes tourists more widely across the island.16 Venice is another example where, prior to the pandemic, cruise ships would dock and disgorge thousands of passengers for day trips. There have been concerns about environmental damage related to the wake of large ships,17 as well as the effect on the city of so many visitors arriving at one time.
The cruise line industry had been growing rapidly prior to the pandemic. The Cruise Line International Association (CLIA) reports that 30 million people globally took a cruise in 2019, and CLIA Australasia estimates approximately 1.35 million Australians and >100,000 New Zealanders took an ocean cruise in 2018.18 However, the public health concern about the high risk of COVID-19 on cruise ships and the role of these ships in spreading the disease led to a crisis, with ships at sea refused permission to dock and outgoing cruises cancelled. A ban was placed on large international cruise vessels entering Australia in March 2020, but this ban expired on 17 April 2022. The Smartraveller website has a useful guide for people planning a cruise, which includes the importance of cruise-specific health insurance. The cruise industry has implemented COVID-19 protocols incorporating testing, vaccination, screening, sanitation, enhanced ventilation, mask wearing, physical distancing and other public health measures by which they plan to mitigate the risk of further outbreaks.19
There is also increasing recognition of the impact of travel on climate change, with the United Nations (UN) World Tourism Agency sponsoring the Glasgow Declaration on Climate Action in Tourism.20 The Declaration now has more than 500 signatories, including major operators such as Expedia Group, Booking Holdings and Condé Nast. The Glasgow Declaration was launched at the UN Climate Change Conference COP26. It is a voluntary commitment, which requests organisations to support halving carbon emissions by 2030 and achieving net zero by 2050 at the latest.
Implications for general practice
A consistent feature of traveller behaviour is that when people do seek pretravel medical advice, it is most often from their general practitioner (GP).21 This implies a responsibility for general practice to have the knowledge, skills and systems in place to provide good-quality health advice and to consider and define their scope of practice. There is currently no widespread consensus on what is in and out of scope for travel medicine in general practice. However, if the GP is not confident that they can adequately conduct risk assessment and provide advice for the traveller due to the complexity of the traveller or destination-specific or itinerary-specific risks, then seeking support or referral is necessary. In some instances, referral is needed to provide specific preventive interventions, such as vaccination for yellow fever or rabies pre-exposure vaccination via the intradermal route.
A defining feature of the practice of travel medicine is risk assessment. This involves an evaluation of the traveller’s health status and medical history, as well as destination-specific risks, including the epidemiology of infectious diseases in the region of travel, and itinerary-specific risks, including length of travel, type of accommodation, urban versus rural travel, modes of transport and higher-risk activities.22,23 Conducting a risk assessment and providing good-quality and comprehensive advice takes longer than the typical primary care consultation, so either breaking up the discussion over more than one consultation or scheduling a longer consultation of at least 20 minutes is necessary. Even after risk assessment is completed, providing appropriate advice takes time. It is therefore necessary for primary care practitioners providing travel medicine services to organise their practices to provide longer consultations for travellers. A preconsultation checklist can be used to collect the key information needed for risk assessment in a structured way while also saving face-to-face consulting time.
Access to and the use of travel health resources for both information and decision support can enhance the quality of practice. Health authorities such as the US CDC, the WHO and the UK National Travel Health Network and Centre (NaTHNaC) provide comprehensive information via their websites.24–26 There are also a number of subscription decision support tools available to provide comprehensive up-to-date, destination-specific and itinerary-specific advice.
Various programs in travel medicine are available, as are opportunities to join professional associations such as the International Society of Travel Medicine, The Royal Australian College of General Practitioners (RACGP) Travel Medicine Specific Interest Group and the Faculty of Travel Medicine of The Australasian College of Tropical Medicine.27–29
Conclusion
GPs need to educate travellers on the increased complexity of international travel, including COVID-19 testing and vaccination requirements, documentation in electronic and hard copy form and travel insurance. Individual risk assessment is more important than ever with re-emerging and emerging diseases and changing models of travel.