Case
An otherwise well girl aged 11 months presented to her general practitioner with an unusual lesion on her posterior neck and was subsequently referred to a dermatologist. The lesion was first noted at six weeks of age and had enlarged a little over time. It was asymptomatic, but the child’s mother reported the lesion had blistered spontaneously on a couple of occasions (Figure 1). These blistering episodes did not cause the child any distress or discomfort and self-resolved without treatment.
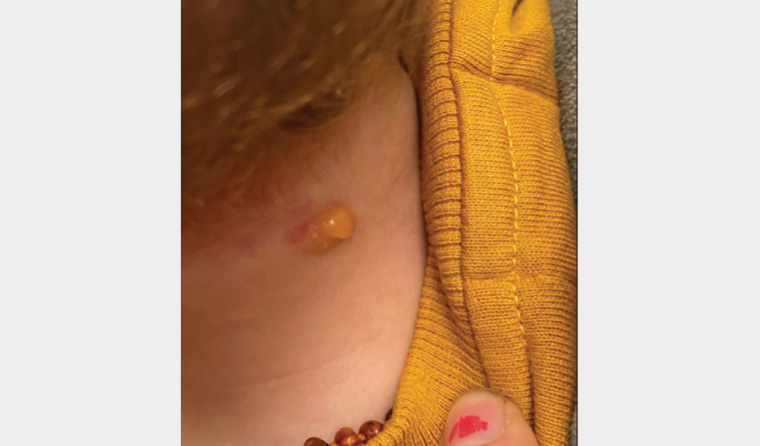
Figure 1. A blistering episode: photograph captured by the patient’s mother, showing a blister overlying the lesion on the posterior neck
On examination, there was an ovoid 14 × 10 mm mildly scaly, yellow-brown plaque on the posterior neck (Figure 2). The lesion had a leathery consistency, and lightly rubbing it did not result in any change in appearance. There was an adjacent erythematous patch consistent with a common benign capillary vascular malformation/naevus simplex.
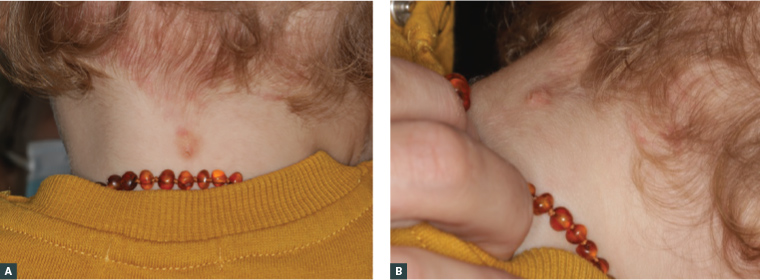
Figure 2. A solitary, mildly scaly, yellow plaque located in the midline on the posterior neck
A. Posterior view; B. Lateral view
Question 1
What is the most likely cause of this condition?
Question 2
What differentials would you consider?
Question 3
How is it diagnosed?
Question 4
How is it managed?
Question 5
What are potential complications?
Answer 1
This case most likely represents a cutaneous mastocytoma. Mastocytomas are a form of mastocytosis. Mastocytoses are a heterogeneous group of disorders characterised by an accumulation of mast cells in tissues.1 Mastocytoses are rare, with an estimated prevalence of 1:10,000.2 They are broadly classified into two groups: cutaneous mastocytosis (CM) and systemic mastocytosis (SM), which also encompass non-cutaneous organ-specific disease.1 CM accounts for 90% of mastocytoses in children3 and has three paediatric subtypes: urticaria pigmentosa, diffuse cutaneous mastocytosis and cutaneous mastocytoma (Table 1).4 Mastocytomas account for 10–15% of paediatric cases of cutaneous mastocytosis and typically present in otherwise well children.5
| Table 1. Classifications of mastocytoses11,12 |
| |
Subtypes |
Description |
| Cutaneous mastocytosis (CM) |
Solitary cutaneous mastocytomas |
10–15% of paediatric CM
A dermal accumulation of mast cells forming 1–3 solitary lesions |
| Urticaria pigmentosa |
(Most common) 70–90% of paediatric CM
Dermal accumulation of mast cells forming four or more solitary lesions ranging from <10 to >100 |
| Diffuse cutaneous mastocytosis |
(Least frequent) 1–3% of paediatric CM
Most severe presentation characterised by diffuse mast cell infiltration in the dermis
Generally associated with systemic manifestations |
| Systemic mastocytosis (SM) |
Extracutaneous mastocytoma |
A benign localised area of mast cell proliferation that is not in the skin
Previously described in the skull and lungs
Often asymptomatic and diagnosed incidentally |
| Includes indolent systemic mastocytosis, smouldering (latent) systemic mastocytosis, aggressive systemic mastocytosis and neoplastic mastocytoses (eg mast cell leukaemia, mast cell sarcoma) |
Multisystem disorders ranging from indolent to aggressive neoplasias
|
Mastocytomas usually present in early infancy.5 They are most common on the trunk and extremities but can appear on any part of the body.6 Typically, they are 1–5 cm in diameter, oval in shape and yellow-brown, and they have a peau d’orange appearance. Lesions may be well demarcated or poorly defined.5 On palpation, they usually feel rubbery or leathery. Up to three mastocytomas may be present. The presence of four or more lesions is considered urticaria pigmentosa.1
Mastocytomas are usually asymptomatic but may be associated with swelling, itching, erythema and occasionally blistering. These changes may occur spontaneously or in response to friction or heat. Rubbing the lesion causes the mast cells to degranulate, releasing histamine, leukotrienes and prostaglandins, which cause a localised urticarial wheal and flare reaction. This is known as Darier’s sign and is particularly associated with cutaneous mastocytoses, although occasionally other conditions, such as scabies, can also show a positive Darier’s sign.7 While Darier’s sign is present on examination in the majority of mastocytoma cases, a negative Darier’s sign does not rule out a mastocytoma.8
In young children with very reactive mastocytomas, eliciting Darier’s sign may provoke flushing and systemic hypotension.1 Thus, caution should be exercised when evoking a Darier’s sign in a patient with multiple or large suspected mastocytomas.
Answer 2
Differentials to consider for yellow-hued cutaneous lesions appearing early in childhood include congenital or early-onset melanocytic naevus, Spitz naevus, xanthoma or juvenile xanthogranuloma and other histiocytoses.6 These conditions will all have a negative Darier’s sign. Differentials to consider for solitary blistering skin lesions in childhood include bullous insect bite reaction, bullous impetigo, allergic contact dermatitis and, less commonly, bullous fixed drug eruption.1 When multiple blistered lesions are present, further differentials to consider are scabies and rare conditions such as epidermolysis bullosa and linear immunoglobulin A bullous dermatosis (Table 2).1
| Table 2. Mastocytoma differential diagnoses |
| |
Yellow lesion |
Blisters |
| Common |
- Congenital melanocytic naevi
|
- Bullous insect bite reaction
- Bullous impetigo
- Scabies
|
| Uncommon |
- Spitz naevi
- Juvenile xanthogranuloma
- Histocytoses
|
- Allergic contact dermatitis
|
| Rare |
|
- Bullous fixed drug eruption
- Linear immunoglobulin A bullous dermatosis
- Epidermolysis bullosa
|
In cases of cutaneous mastocytoma, it is important to exclude more widespread disease. A full skin examination should reveal three or fewer lesions. Widespread cutaneous mastocytosis can be associated with systemic mastocytosis, symptoms of which may include episodic flushing, dyspnoea, hypotension, nausea, vomiting, abdominal pain, diarrhoea and headaches.5
Answer 3
Mastocytomas can be diagnosed by the typical clinical history and examination findings, which usually include the presence of a positive Darier’s sign. A biopsy is usually not necessary unless there is diagnostic uncertainty. If there is diagnostic uncertainty, a small punch biopsy (3 mm) is optimal. Histopathology will demonstrate a dermal infiltrate of mast cells, particularly in the papillary dermis, and is often accompanied by dermal oedema and eosinophils.3 Mast cells are best visualised using special stains such as Giemsa and toluidine blue.9
Laboratory and radiological investigations are not usually required unless there are multifocal lesions and concerns regarding systemic symptoms.5
Answer 4
Treatment is largely symptomatic. Parents can be reassured regarding the benign nature and that the lesion will most likely resolve in time. Trauma and excoriations to the lesion and exposure to heat should be minimised to avoid provoking itch, swelling and blistering. Oral H1-antihistamines, such as loratadine, cetirizine, fexofenadine, are helpful for symptomatic cases of pruritis and flushing. Topical corticosteroids such as methylprednisolone aceponate and mometasone furoate, with or without occlusion, are useful in the treatment of inflammation and pruritis associated with lesion flaring.3,5
If there is diagnostic uncertainty, presence of multiple cutaneous lesions or reports of systemic symptoms, then patients should be referred for specialist paediatric dermatological assessment. Multidisciplinary management may be required.
Answer 5
Mastocytomas generally follow a benign course. Usually, the lesion will increase in size for several months, after which it grows proportionally with the child. This is followed by a gradual resolution, usually without scarring, over a variable time course.5 Most cases that present in a child less than two years of age will generally have resolved by puberty.10
Rarely, paediatric mastocytoma may present with symptoms of acute mast cell activation, including anaphylaxis.5,11 Any child with systemic symptoms such as whole-body flushing, shortness of breath, wheezing, nausea, vomiting, diarrhoea or hypotension should be referred for further assessment. An individual risk assessment and treatment plan can then be determined, which in a small number of cases may include the prescription of adrenaline injector pens and recommendation for a medical ID bracelet.
Key points
- Cutaneous mastocytomas can be diagnosed clinically through history and examination findings, which usually include a positive Darier’s sign.
- The majority of mastocytomas in children presenting before two years of age will spontaneously resolve.
- Atypical cases or those presenting with features suggestive of more widespread or systemic disease should be referred for specialist paediatric dermatological assessment.