Case
A woman aged 39 years presented with a 12-year history of recurrent painful nodules and boils to the axillae and pubic areas. On examination of the axilla (Figure 1), she was noted to have multiple tender inflamed nodules and extensive scarring. Pus was able to be expressed from two sinus tracts. Examination of the lower pubic region (Figure 2) revealed similar findings.
She reported a significant impact on her quality of life and associated psychological burden owing to her condition. She also described significant pain, which fluctuated in severity according to the number of active lesions. Thick bands of chronic scarring to the axilla had led to decreased mobility of her arms.
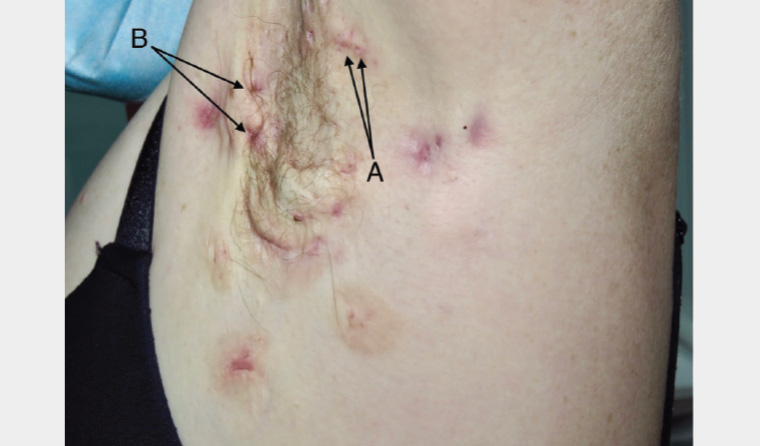
Figure 1. Hidradenitis suppurativa to the left axilla demonstrating Hurley Stage 2.
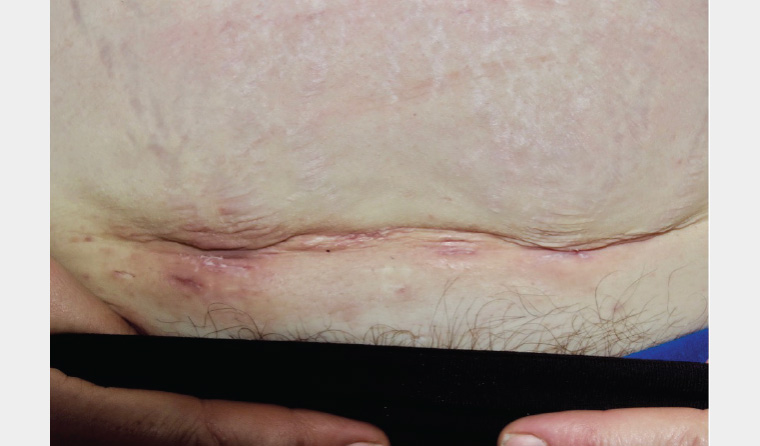
Figure 2. Hidradenitis suppurativa to the lower abdomen
Question 1
What diagnoses would you consider?
Question 2
Who is most likely to develop hidradenitis suppurativa?
Question 3
How is hidradenitis suppurativa diagnosed?
Question 4
What is Hurley staging?
Question 5
How is hidradenitis suppurativa managed?
Answer 1
The most likely diagnosis is hidradenitis suppurativa. Differential diagnoses include staphylococcal skin infections, furuncles, carbuncles and abscesses, but these are unlikely to present with this prolonged time course and degree of scarring. Cutaneous Crohn’s disease is another differential diagnosis. However, this generally presents with skin tags, oedema and fissures in addition to abscesses. It is predominantly found around the perineal and perianal area, as opposed to axilla and groin as in this case.
Hidradenitis suppurativa is a chronic auto-inflammatory skin disease of hair follicles associated with inflamed cutaneous nodules, abscesses and malodorous pus-discharging sinuses. These lesions generally form in the intertriginous regions, such as the axillary, inguinal and gluteal skin folds, but can develop anywhere on the body.1 Hidradenitis suppurativa was previously thought to be a disease of the apocrine glands because of the regions of the body typically affected. Intertriginous sites are now thought to be involved because of heat and friction in these areas.1
Hidradenitis suppurativa nodules form when the hair follicle becomes blocked by keratin.1 The resulting inflammatory response results in rupture of the hair follicle, which spreads inflammatory cytokines into the local tissues. This, in turn, worsens the local inflammation.1 Sinus tracts can form between active lesions, which may continue chronically discharging malodourous fluid.
Scarring, physical disfigurement and associated significant pain can be extensive and frequently have a major adverse effect on quality of life.2 An Australian population study with a validated hidradenitis suppurativa screening questionnaire revealed that approximately 25% of patients with symptoms suggestive of hidradenitis suppurativa have never sought medical help.3 Barriers to accessing care include embarrassment and stigma.4 The average time from first symptoms to diagnosis is 10 years.5
The general practitioner is well placed to recognise and diagnose hidradenitis suppurativa. Patients presenting with recurrent boils or abscesses in the intertriginous zones should prompt consideration of hidradenitis suppurativa.
Answer 2
Approximately one in every 150 people in Australia has hidradenitis suppurativa.3 Hidradenitis suppurativa is three times more common in women than men6 and tends to begin at or just after puberty.2 One in three people with hidradenitis suppurativa has a family history.6
Hidradenitis suppurativa is particularly associated with, and worsened by, smoking.7 There is also an association with metabolic syndrome, spondyloarthropathy and inflammatory bowel disease.8
Answer 3
Hidradenitis suppurativa is a clinical diagnosis and should be considered in patients presenting with painful boils and abscesses preferentially affecting the armpits, genitals and groin.
Pseudocomedones (Figure 1, Point A), also termed double-headed comedones or polyporous comedones, are a key diagnostic feature that may also be seen on examination.1
Answer 4
Hidradenitis suppurativa varies significantly in severity between individuals, with the majority having mild-to-moderate disease.6 Assessment of severity can aid in referral and selection of appropriate treatment modalities. The most well-known staging system for severity is Hurley staging (Table 1).9
| Table 1. Hurley staging in hidradenitis suppurativa |
| Hurley staging |
Description |
| Stage 1 (Mild) |
Abscess formation (single or multiple) without sinus tracts |
| Stage 2 (Moderate) |
Recurrent abscesses with sinus tracts and scarring |
| Stage 3 (Severe) |
Diffuse or almost diffuse involvement or multiple interconnected tracts and abscesses |
Answer 5
Treatment is complex and multifactorial, and it should be tailored to the individual.
Conservative measures play an important part and should address comorbidities, especially smoking, obesity and activity levels. Antiseptic washes, loose-fitting or anti-chafing clothing and control of perspiration are additional valuable preventive measures.7
Much of the pain in hidradenitis suppurativa is caused by pressure from an abscess. Early and adequate drainage can give quick pain relief. Intralesional steroids can be considered for persistently painful lesions. Compounded 15% topical resorcinol is a useful adjunct and acts as a drawing agent for active boils.10
Many patients also benefit from daily topical antibiotic therapy (eg clindamycin lotion).8 Some women may also report improvement with anti-androgenic oral contraceptives.7 Long-term antibiotics (eg doxycycline or erythromycin) may be used for their anti-inflammatory action. Hidradenitis suppurativa abscesses start as a purely inflammatory lesion where culture of the pus is sterile.7 As such, antibiotics will not treat an infection nor give pain relief.
For more severe disease, deroofing surgery with healing by secondary intention may have a role.11 Immunomodulatory therapies such as adalimumab may be of benefit.7 Early referral should be considered for patients who may benefit from these measures.
Mental healthcare is an essential component of hidradenitis suppurativa management, as hidradenitis suppurativa is associated with higher odds of having depression, anxiety, bipolar disorder, personality disorders, substance-related disorders, alcohol abuse and schizophrenia.12
Hidradenitis suppurativa has been described as one of the most painful dermatological conditions.13 Optimisation of analgesia is paramount.
Case continued
This patient’s condition was found to be refractory to multiple therapies. She is currently participating in a clinical trial investigating the role of a new immunomodulatory therapy in managing hidradenitis suppurativa.
Key points
- Hidradenitis suppurativa is a chronic auto-inflammatory skin disease of hair follicles.
- Hidradenitis suppurativa is a clinical diagnosis and should be considered in patients presenting with painful boils and abscesses.
- Management is multifactorial and should be tailored to the individual.