Nature prescribing can be facilitated through referrals to external providers, online or through link workers. Nature-based activities could be incorporated into chronic disease management plans, mental health care plans and National Disability Insurance Scheme plans.
Nature prescribing can be beneficial for people of all ages, and especially for people with chronic disease and/or mental health conditions. Spending time in nature may provide additional benefits, including social connection and connection to the environment.
Nature prescribing involves a health professional giving patients a recommendation to spend time in nature, and may also encompass written prescription, verbal counselling or referral to another provider.1 Nature prescribing may include prescribing nature-based activities that enhance physical activity and improve social connection, wellbeing and mental health. Nature therapy is sometimes referred to as ecotherapy, forest bathing or forest therapy.
Nature prescribing builds on humans’ biophilia (love of natural environments)2 and a well-developed general framework for restorative environments.3 It may be useful for the prevention of and therapy for chronic physical and mental health conditions. Contact with nature may constitute a preventive, ‘upstream health promotion intervention for populations’.4
The chronic disease burden in Australia is considerable and growing. In 2017–18, more than 11 million Australians (47%) had one or more of the 10 most common chronic conditions (including diabetes, mental health conditions, cardiovascular disease, cancer, asthma, arthritis and chronic obstructive pulmonary disease).5 Sedentary lifestyles, poor diet and an ageing population further aggravate risks of these conditions.
Nature prescribing can intersect with social prescribing in that both shift the focus from illness to wellness, enable consumer self-management and decrease a felt sense of helplessness, decrease loneliness and strengthen communities.6 The Consumer’s Health Forum of Australia and The Royal Australian College of General Practitioners (RACGP) 2019 roundtable strongly supported the use of social prescribing in primary care.6
Aim
The aim of this article is to provide guidance on the implementation of nature prescribing in general practice.
Evidence for nature prescribing
Although much research has been conducted in Australia and overseas on the benefits of contact with nature,7 evidence from international randomised trials of the effectiveness of nature prescriptions is limited.8 Table 1 shows the types of green and blue space interventions.
‘Green space’ nature therapy
‘Green space’ interventions are delivered in land-based natural environments. Such interventions can include walking or running in parkland, bushwalking, cycling, gardening or farming, animal or wildlife care, nature art, craft or writing or wilderness sports, or simply ‘being’ in green environments (shinrin-yoku, or forest bathing).
Parkrun, a five kilometre walk or run, is an example of a green space activity.9 Parkrun is hosted in over 2000 sites around the world, with some clinicians already recommending it to patients because it is low-cost and accessible for those with low fitness.
Kondo et al1 conducted a narrative review of case studies and empirical studies that discussed outdoor interventions initiated by health professionals and reviewed 11 studies. Although the quality of studies was poor and no clear physical health or wellbeing outcomes were identified, the review showed that interventions were feasible, including in community health centres (two studies).1 The interventions varied in time intensity, ranging from daily to weekly outdoor programs. Unstructured nature prescribing was also assessed (eg recommending walks in local parks or national parks), with incentives such as free passes or motivators such as pedometers or exercise diaries.1
A scoping review with nested meta-analysis of nature prescribing conducted by Nguyen et al10 included randomised and non-randomised controlled studies of nature prescribing (86 studies in total). Compared with controls, nature prescription programs resulted in greater reductions in systolic blood pressure (mean difference [MD] –4.9 mmHg [95% CI: –9.6, –0.1 mmHg]; I2=65%) and diastolic blood pressure (MD –3.6 mmHg [95% CI: –7.4 to 0.1 mmHg]; I2=67%) after the intervention, showing that these programs may be an adjunct to pharmacotherapy. Nature prescribing may help people meet physical activity recommendations. The RACGP Red Book11 recommends that people aged 18–64 years undertake 150–300 minutes of moderate-intensity physical activity, along with strength or toning on at least two days per week; however, only 24.5% of people aged 18–64 years meet these physical activity guidelines.11,12 The review by Nguyen et al showed how nature prescriptions led to greater increases in daily step counts (MD 900 steps [790, 1010]; I2=0%).10 Physical activity in natural environments is also likely to result in less exposure to air pollution and heat.
Spending time in nature can offer other benefits apart from physical activity, including social connection and improvement in wellbeing indicators, such as reduced depression scores (standardised MD [SMD] 0.5 [0.2, 0.8]; I2=79%) and anxiety scores (SMD 0.6 [0.1, 1.2]; I2=90%).1,10 Emerging evidence indicates that these psychological benefits may be closely entwined with restorative processes that ameliorate feelings of chronic loneliness.13
Only one study has been conducted in general practice in Australia, in Adelaide.14 This study involved an 8-week facilitated nature prescribing trial, first mapping green spaces locally, followed by the recruitment of 30 general practitioners (GPs) who recruited participants with chronic disease (mild–moderate diabetes or depression/anxiety). General wellbeing (measured using the Kessler Psychological Distress Scale [K10]) improved from the start to the end of the trial (mean [± standard deviation] 37.3 ± 3.53 vs 56.3 ± 8.41, respectively; n = 3), with nature connectedness also increasing. The study was hampered by its small sample size (n = 6 participants).14
‘Blue space’ nature interventions
‘Blue’ nature therapy includes interventions in or in the vicinity of water, including streams, rivers, lakes or the ocean,15,16 and can include surfing, dragon boat racing, scuba diving, sailing, fishing, swimming and walking or running by rivers or the sea. A systematic review by Britton et al included 33 studies assessing the effect of blue space interventions aimed at improving health and wellbeing.16 Most of the included papers found a positive or weak association with wellbeing, with evidence of greater social connectedness also reported, although a meta-analysis was not possible. The results were mixed for indicators of physical wellbeing.16 More research is required regarding the health effects of blue-space interventions.
Role of primary care teams
In the review of Kondo et al, GP leaders or ‘clinician champions’ played a critical role in supporting nature programs, promoting engagement and liaising with the nature providers.1 Practice nurses, Aboriginal Health Workers and other primary care health professionals may also lead programs.
Social prescribing may be particularly effective if a health professional refers patients to a ‘link worker’ (or community health worker) who can provide coaching and connections to a range of resources, supplementing the health practitioner’s focus on biomedical options.17 Some primary health networks (PHNs) fund such link workers. Local online resources, such as HealthPathways supported by PHNs, or local government websites may list providers of nature-based activities, along with other social prescribing activities.
Nature prescribing in practice
In the past, the Lifescripts program included paper ‘scripts’ for dietary advice and physical activity;18 however, verbal advice or referrals to other services can also be used for nature prescribing. Prescriptions, whether written or verbal, could include the type of activity, frequency and duration of activity (eg community gardening, once a week, for a month).
Nature prescribing can be integrated opportunistically into advice on physical activity.6 Medicare Benefits Schedule-funded health checks for people aged 45–49 years, the elderly, those with an intellectual disability and for Aboriginal and Torres Strait Islander people are an ideal time to discuss physical activity.
Nature-based activities can be written into chronic disease care plans and team care arrangements (eg as part of diabetes management). Figure 1 shows nature interventions. Nature prescribing could be incorporated into mental healthcare plans for those with conditions such as depression or chronic schizophrenia.19

Figure 1. Types of nature-based interventions.
Enhanced primary care arrangements can be used to access allied health professionals with an interest in this area (eg occupational therapists). Shared medical appointments have been used to support other lifestyle interventions20 and could be used to support programs run by GPs themselves. National Disability Insurance Scheme (NDIS) plans can also support those with disabilities, with specialist nature intervention providers available.
Matching of activities with clinical condition
Primary care teams know both the person and local networks of services. Each person will have their own preference for activities, and this needs to align with factors such as location, cost, motivation, age of peers and preference for individual or group activities. GPs may also need to consider the health condition and the physical or cognitive ability required for each activity.
Age, gender or culturally specific group activities may also facilitate connection to community (eg Aboriginal walking or marathon groups). Involvement in programs may increase understanding of Aboriginal connection to country.14
Options for nature prescribing may also be located in online social prescribing resources, such as HealthPathways or other agencies (eg https://adma.org.au/social-prescribing-initiatives, accessed 1 March 2023; Figure 2).
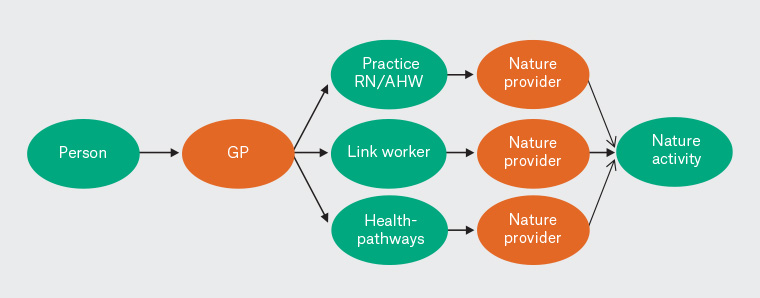
Figure 2. Referrals to nature providers.
AHW, Aboriginal Health Workers; GP, general practitioner; RN, registered nurse.
Facilitators and barriers
Facilitators to participation include being free or low cost, local and enjoyable, and supporting weight loss.1
Lack of time, transport or resources were reported as barriers to participation in nature-based prescribed activities in one review.1 Poor weather (excesses of heat and cold, or rain) may be a disincentive to participate in outdoor activities,21 and may carry risks for frailer or older participants. Other potential risks of outdoor activities include sunburn, dehydration, trip or falls, insect bites, bushfires, interaction with wild animals22 or infection.23 Blue zone or water-based activities may be associated with an increased risk of drownings24 or marine stings. An active approach to anticipating and preventing negative impacts is advised.
Other considerations may include perceived safety in outdoor locations, lighting and quality of pathways or access. Those of lower socioeconomic status may live further from green and blue spaces (parks, gardens, bush, lakes, rivers or the ocean),25 and may be less likely to have transport to access such areas.
Broader public health campaigns to promote nature-based activities are critical; primary care-based programs can support broader interventions. For example, local councils and state governments may increase the number of parks, support the greening of communities and active transport, and support community gardens. Many organisations can promote nature-based activities, including schools and preschools, hospitals and residential aged care facilities (eg ‘healing gardens’). General practices may also set up a community garden.
Some nature-based activities may have benefits for the environment itself (eg bush regeneration, wildlife rescue or community gardening), which can be useful in those with climate–change-related anxiety. Clinicians themselves may find that spending time in natural environments prevents burnout or provides a therapeutic effect.
Conclusion
Nature prescribing is likely to increase physical activity and improve mental and cardiovascular health outcomes. Nature prescribing can be incorporated into prevention programs, as well as chronic disease and mental health management in general practice.
Key points
- Nature prescribing involves recommending time in nature.
- Time in green or blue space is associated with improvements in physical and mental wellbeing.
- Facilitators include the availability of low-cost or free activities, and the use of link workers.
- Nature-based interventions could be incorporated into chronic disease management plans, mental healthcare plans and National Disability Insurance Scheme plans.
- Further research is needed to confirm the health benefits of nature prescribing.