In Australia, cardiovascular disease (CVD) is the leading cause of death and accounts for 9% of total disease expenditure ($10.4 billion).1,2 If current Australian guidelines were fully implemented, using absolute CVD risk assessment to guide the prescribing of medication for high-risk patients, an estimated $5.4 billion would be saved per year.3,4 MedicineInsight data suggest that only 17% of Australian patients aged 45–74 years attending general practice have the required risk factors recorded to enable an absolute CVD risk assessment, although this may not be representative and is limited to data recorded in specified fields.5
Health assessment Medicare Benefits Schedule (MBS) items are time-based consultation items targeted towards the prevention and management of chronic diseases that include taking a patient’s history, physical measurements and providing management advice about medication and lifestyle change (Table 1). To increase the uptake of CVD primary prevention guidelines, a dedicated ‘Heart Health Check’ MBS item (699) was introduced on 1 April 2019, under which medical practitioners could claim a fee ($85.60) for a dedicated CVD risk consultation that lasts at least 20 minutes.6 Item 699 has a specific focus on identifying CVD risk factors and initiating CVD risk management strategies for high-risk patients. However, Item 699 cannot be claimed if any of the existing health assessment items have been claimed in the previous 12 months. As such, it is possible that the introduction of Item 699 may be a competing factor that detracts from the use of other health assessment items.
| Table 1. Overview of Medicare Benefits Schedule health assessment items and conditions for claiming for the general population |
| |
Fee ($) |
Consultation time (minutes) |
Patient history |
Physical examination |
Management requirements |
Frequency of service |
Target population |
| Item 699: Heart health assessment |
75.05 |
>20 |
Patient history, including CVD risk factors (diabetes status, alcohol intake, smoking status) |
Blood pressure
Cholesterol status
Blood glucose |
Initiate interventions and referrals for identified risk factors
Implement management plan
Provide preventative healthcare advice |
Once per 12 months |
Patients with CVD or at risk of developing CVD |
| Item 701: Brief health assessment |
61.20 |
≤30 |
Patient history as required |
Basic physical examination |
Initiate interventions and referrals
Provide preventive healthcare advice and information |
Provided annually to an eligible patient depending on patient comorbidities |
Not specified |
| Item 703: Standard health assessment |
142.20 |
>30–44 |
Detailed patient history |
Extensive physical examination
|
Initiate interventions and referrals
Provide a preventative healthcare strategy |
Up to annual depending on patient comorbidities |
Patients without complex health issues |
| Item 705: Long health assessment |
196.25 |
45–59 |
Comprehensive patient history |
Extensive examination of medical condition and physical function |
Initiate interventions and referrals
Provide a basic preventative healthcare management plan |
Up to annual depending on patient comorbidities |
Patients with a range of health issues |
| Item 707: Prolonged health assessment |
277.20 |
>60 |
Comprehensive patient history |
Extensive examination of medical condition and physical, psychological and social function |
Initiate interventions and referrals
Provide a comprehensive preventative healthcare management plan |
Up to annual depending on patient comorbidities |
|
| Item 715: Health assessment for Aboriginal and Torres Strait Islander peoples |
218.90 |
Not stated |
Patient history* |
Examinations and investigations as required* |
Initiate interventions and referrals
Provide advice and information* |
Once per 9 months |
Aboriginal and Torres Strait Islander peoples |
| *Assessment advice changes for each target population, including children aged <15 years, adults aged 15–54 years and older people aged >55 years. CVD, cardiovascular disease. |
From April 2020 there have been multiple changes to the delivery of primary health services in response to the COVID-19 pandemic.7 Despite effective COVID-19 control measures in Australia, national general practitioner (GP) surveys conducted in 2020 and 2021 indicated a high impact of and concern about the pandemic, including the safety of staff, the rapid move to telehealth, reduced income due to a drop in patient presentation, increased workload during the vaccination rollout and inadequate government support, including a lack of safety equipment.8,9 In addition, the National Heart Foundation of Australia has estimated that 27,000 fewer Heart Health Checks were conducted due to COVID-19.10 As such, this study aimed to explore the uptake of Item 699 since its introduction and changes in existing health assessment item claims. In addition, this study examined the change in health assessment item claims for the 12-month period before and after COVID-19 pandemic outbreaks started impacting health service delivery and patient presentation to GPs.
Methods
Study overview
Publicly available databases were used for MBS item claims and population estimates.11 Data were available by age range, sex and state or territory. Because it was not possible to determine race or ethnicity, data for all adults aged ≥35 years were included in accordance with national guideline recommendations at the time of data collection for absolute CVD risk assessment in Aboriginal and Torres Strait Islander people aged ≥35 years and all other adults aged ≥45 years.3 MBS claims data for health assessment Items 699, 701, 703, 705, 707 and 715 were downloaded and compared between three time periods: the 12-month period before the introduction of Item 699 (1 April 2018–31 March 2019); the 12-month period after the introduction of Item 699 (1 April 2019–31 March 2020); and the 12-month period with COVID-19 outbreaks affecting the delivery of health services through primary care (1 April 2020–31 March 2021).12 Subsequently, health assessment item claims were assessed by age, sex and state/territory for the 24-month period after Item 699 was introduced (1 April 2019–31 March 2021). Only MBS health assessment items claimed by GPs were included in the analyses because health assessment Items 701–707 require GP presence.
Data access
MBS Online was used to obtain MBS health assessment item claim data from the ‘Medicare Items Statistics Reports’ webpage.11 Data were available in aggregate and downloaded per quarter to analyse uptake over time. Data were extracted on 26 July 2021.
Overview of MBS health assessment items
The MBS health assessment items consist of four time-based items, namely 701 (brief), 703 (standard), 705 (long) and 707 (prolonged) consultations, with Item 715 specifically for health assessment among Aboriginal and Torres Strait Islander individuals.3 Item 699 includes the same basic requirements as the existing health assessment items but with a focus on identifying CVD risk factors, including blood pressure measurement, and initiating CVD risk-reduction interventions.
Data analysis
Data were analysed using STATA version 16.1 (StataCorp, College Station, TX, USA). Descriptive analysis was conducted on the number of MBS claims nationally for health assessment Items 699, 701, 703, 705, 707 and 715 according to the absolute number of claims by age, sex and state.
Results
Health assessment item claims in Australia before and after the introduction of Item 699
Figure 1 presents an overview of the trends in MBS health assessment items claims over the study period. Table 2 details the change in health assessment item claims from before to after the introduction of Item 699, including a 12-month period with COVID-19 restrictions. Item 699 accounted for 9.4% of all health assessment item claims (175,214 claims) during the 24 months since its introduction. The health assessment item with the longest consultation time, Item 707, accounted for the most claims during the 24 months after the introduction of Item 699 (697,729 [37.3%] of all health assessment item claims). Overall, claims for existing health assessment items were virtually unchanged, with an increase of 1.4% in the 12 months after Item 699 was introduced compared with the 12 months before Item 699 was introduced (Table 2). Claims for the shortest health assessment, Item 701, had the greatest relative decrease (12.2%) in the 12 months after Item 699 was introduced (absolute decrease of 3900 claims).
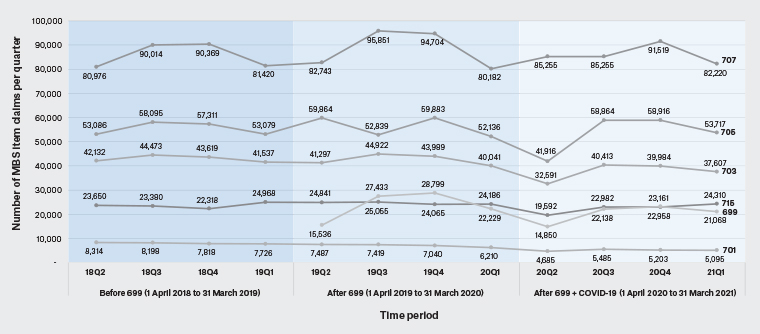
Figure 1. Medicare Benefits Schedule (MBS) health assessment item claims before and after the introduction of the Heart Health Check Item 699 among Australian adults aged ≥35 years. Data are presented for health assessment item claims for three 12-month periods: before Item 699 (‘Before 699’) was introduced, the first 12 months after Item 699 was introduced (‘After 699’) and the 12-months after COVID-19 pandemic restrictions were introduced (‘After 699 + COVID-19). Item claims are shown quarterly (Q1–Q4) for 2018 (18), 2019 (19), 2020 (20) and 2021 (21). Click here to enlarge.
|
Table 2. Health assessment item Medicare Benefits Schedule claims before and after the introduction of Heart Health Check Item 699
|
|
|
MBS health assessment item
|
All health assessment items
|
|
699
|
701
|
703
|
705
|
707
|
715
|
|
Total number of claims n (% of total claims)
|
|
Period 1: 12-month period before introduction of Item 699 (1 April 2018–31 March 2019)
|
|
Total no. claims per item
|
–
|
32,056
|
171,761
|
221,571
|
342,779
|
94,316
|
862,483
|
|
Mean no. claims per quarter
|
–
|
8,014
|
42,940
|
55,393
|
85,895
|
23,579
|
215,621
|
|
Proportion of claims in period (%)
|
–
|
3.7
|
19.9
|
25.7
|
39.7
|
10.9
|
–
|
|
Period 2: 12-month period after introduction of Item 699 (1 April 2019–31 March 2020)
|
|
Total no. claims per item
|
93,997
|
28,156
|
170,249
|
224,722
|
353,480
|
98,147
|
968,751
|
|
Mean no. claims per quarter
|
23,499
|
7,039
|
42,562
|
56,181
|
88,370
|
24,537
|
218,689
|
|
Proportion of claims in period (%)
|
9.7
|
2.9
|
17.6
|
23.2
|
36.5
|
10.1
|
–
|
|
Period 3: 12-month period with Item 699 and COVID-19 restrictions (1 April 2020–31 March 2021)
|
|
Total no. claims per item
|
81,217
|
20,486
|
150,595
|
213,413
|
344,249
|
89.842
|
899, 784
|
|
Mean no. claims per quarter
|
20,304
|
5,117
|
37,649
|
53,353
|
86,062
|
22,461
|
204,642
|
|
Proportion of claims in period (%)
|
9.0
|
2.9
|
16.7
|
23.7
|
38.3
|
10.0
|
–
|
|
Difference in number of claims between different periods
|
|
Period 1 vs Period 2
|
|
Change in total no. item claims
|
|
–3,900
|
–1,512
|
3,151
|
10,701
|
3,381
|
12,271†
|
|
Change in mean no. item claims
|
–
|
–975
|
–378
|
788
|
2,675
|
958
|
3,068
|
|
% Change in claims*
|
–
|
–12.2
|
–0.9
|
1.4
|
3.1
|
4.1
|
1.4
|
|
Period 2 vs Period 3
|
|
Change in total no. item claims
|
–12,780
|
–7,688
|
–19,654
|
–11,309
|
–9,231
|
–8,305
|
–68,967
|
|
Change in mean no. item claims
|
–3,195
|
–1,922
|
–4,914
|
–2,827
|
–2,308
|
–2,076
|
–14,047
|
|
% Change in claims*
|
–13.6
|
–27.3
|
–11.5
|
–5.0
|
–2.6
|
–8.5
|
–7.1
|
|
*The percentage difference was taken as the difference in the number of claims as a proportion of total claims per item or of the total in the previous period. †Total claims excluding Item 699 to make a direct comparison for claims for all health items before and after the introduction of Item 699. MBS, Medicare Benefits Schedule.
|
Claims for all health assessment items decreased by 7.1% in the 12 months after COVID-19 restrictions were introduced compared with the previous 12 months, with 68,967 fewer claims. The health assessment items with the shortest consultation times had the greatest relative reduction in claims in the 12 months with COVID-19 restrictions compared with the previous 12-month period (Item 701: 27.3% decrease, 7,688 fewer claims; Item 703: 11.5% decrease, 19,654 fewer claims). Item 699 had a 13.6% relative reduction in claims during the 12 months with COVID-19 restrictions, with 12,780 fewer claims than the first 12 months the item was available.
Health assessment item claims by age range
Table 3 details health assessment item claims by age range. Item 699 had the greatest claims for those aged 55–74 years, accounting for 66% of all Item 699 claims, and 48% of all health assessment item claims among this age range. Those aged ≥75 years accounted for 64% of all health assessment item claims, with the long and prolonged consultations, namely Items 705 and 707, the most claimed items among this group, accounting for 55% and 59% of total item usage for both items, respectively.
|
Table 3. Medicare Benefits Schedule health assessment item claims by age category among adults aged ≥35 years in the 24 months after Item 699 was introduced (1 April 2019–31 March 2021)
|
|
|
Age (years)
|
Total no. claims
per item
|
|
35–44
|
45–54
|
55–64
|
65–74
|
≥75
|
|
MBS Item
|
|
|
|
|
|
|
|
699
|
10,042 (6)
|
43,829 (25)
|
63,213 (36)
|
52,739 (30)
|
5,391 (3)
|
175,214 (10)
|
|
701
|
9,513 (20)
|
16,444 (34)
|
1,758 (4)
|
1,449 (3)
|
19,460 (28)
|
48,624 (3)
|
|
703
|
21,222 (7)
|
76,578 (24)
|
5,908 (2)
|
8,090 (3)
|
209,046 (46)
|
320,844 (17)
|
|
705
|
12,443 (3)
|
65,951 (15)
|
5,380 (1)
|
9,344 (2)
|
345,017 (55)
|
438, 135 (24)
|
|
707
|
7,607 (1)
|
45,690 (7)
|
6,602 (1)
|
14,710 (2)
|
592,692 (59)
|
667,301 (36)
|
|
715
|
51,141 (27)
|
55,682 (30)
|
45,718 (24)
|
25,683 (14)
|
9,765 (4)
|
187,989 (10)
|
|
Total no. claims per item
|
111,968 (6)
|
304,174 (17)
|
128,579 (7)
|
112,015 (6)
|
1,181,371 (64)
|
1,838,107 (100)
|
|
Data show the number of Medicare Benefits Schedule (MBS) health assessment item claims by age range, with percentages (of total claims per item) in parentheses.
|
Health assessment item claims by sex
Figure 2 shows MBS health check item usage by sex over the 24-month period after Item 699 was introduced (1 April 2019–31 March 2021). Women accounted for 54% of all health assessment item claims, with 161,555 more health assessment item claims than men (women, 998,941 claims; men, 837,386 claims). Women had more claims for the health assessment items with longer consultation times than men (Item 705: 232,975 vs 201,218 claims, respectively [difference = 31,757 claims]; Item 707: 380,786 vs 288,677 claims, respectively [difference = 92,109 claims]). The absolute number of Item 699 claims was higher among men than women, with 1,516 more items claimed for men than women, but the relative difference was only 0.01%.
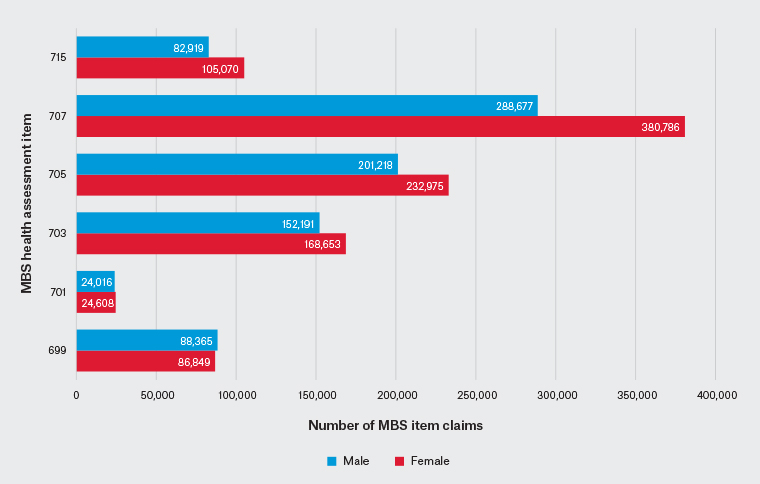
Figure 2. Use of Medicare Benefits Schedule (MBS) health assessment items by sex over the 24 months after Item 699 was introduced (1 April 2019–31 March 2021) among adults aged ≥35 years. Click here to enlarge.
Health assessment item claims by state or territory
New South Wales, Queensland, and Victoria had the greatest absolute claims for Item 699 (56,384, 43,685 and 34,730, respectively; Table 4). However, the number of claims relative to the population was similar across states and territories, ranging from 0.8% to 1.6%. Tasmania and the Northern Territory had the lowest absolute and relative claims of Item 699 (2,457 and 996 claims, 0.8% and 0.9% of the population, respectively). Queensland and Western Australia had the highest proportion of Item 699 claims relative to population, at 1.6% each.
|
Table 4. Medicare Benefits Schedule health assessment Item 699 claims by Australian state or territory in the 24 months after Item 699 was introduced (1 April 2019–31 March 2021)
|
|
State or territory
|
Population
|
No. Item 699 claims
|
Item 699 claims (% population)
|
|
New South Wales
|
4,438,535
|
56,384
|
1.3
|
|
Victoria
|
3,523,887
|
34,730
|
1.0
|
|
Queensland
|
2,751,350
|
43,685
|
1.6
|
|
Western Australia
|
1,416,907
|
22,735
|
1.6
|
|
South Australia
|
1,019,036
|
13,701
|
1.3
|
|
Tasmania
|
320,016
|
2,457
|
0.8
|
|
Australian Capital Territory
|
217,444
|
2,469
|
1.1
|
|
Northern Territory
|
115,177
|
996
|
0.9
|
Discussion
In this nationwide study, the new ‘Heart Health Check’ Item 699 accounted for 9.4% of all health assessment item claims since its introduction, without a corresponding decline in claims for existing health assessment items. Claims for all health assessment items declined during the first 12 months of the COVID-19 pandemic outbreak. Health assessment items with the shortest consultation times and Item 699 had the greatest decline in claims during this period. Item 699 was the most used health assessment item among patients aged 55–74 years. Overall, these findings suggest promising initial uptake of Item 699, particularly among those aged 55–74 years, in whom absolute CVD risk assessment is recommended according to CVD primary prevention guidelines. It is important to note that MBS claims may not match GP data if the CVD risk assessment is not adequately recorded in medical records, or if different item numbers are used. So, the actual use of CVD risk assessment tools may be higher or lower than indicated by the data presented in this paper.
Hypertension and dyslipidaemia are among the most prevalent conditions recorded during GP consultations.13 In 2020, national data indicated that 49% of patients aged 45–74 years had the requisite CVD risk factors for absolute CVD risk assessment (smoking status, diabetes status, blood pressure and lipid levels) recorded in their GP record.13,14 However, these data do not elucidate whether absolute CVD risk assessment was undertaken as per guideline recommendations. Indeed, data demonstrate that <10% of patients aged 45–74 years have an absolute CVD risk score in their GP record.15 Together, these data support existing evidence that GPs favour a single risk factor management approach rather than absolute CVD risk.16,17 This disconnect between guideline recommendations and CVD risk management in practice was the rationale for the introduction of Item 699, yet absolute CVD risk assessment is not stipulated as a requirement to claim the item. Embedding absolute CVD risk assessment as a requirement to claim Item 699 may ensure guideline-recommended use of absolute CVD risk rather than single risk factor management. Indeed, Item 699 claims were predominantly among those aged 45–74 years and Item 699 was the most used item among those aged 55–74 years, a group with low claims for pre-existing health assessment items. Item 699 has likely created a designated opportunity to collect CVD risk factor information among those aged 45–74 years, where there was previously a gap, and such activity was undertaken opportunistically in primary care.16,18,19
The use of MBS services fell by 10% nationally in April 2020 in response to the COVID-19 pandemic outbreak.12 In the present study, Item 699 had the greatest decline of all health assessment items during this period. Due to the COVID-19 outbreak and associated public health response, there have been multiple changes to primary care delivery, including a rapid move to telehealth and fewer patient presentations.8,9 The decline in Item 699 may reflect its recent introduction (and thereby being among the first to be dropped) or, more likely, the challenge of collecting CVD risk factor information remotely, including blood pressure, which is a requirement for Item 699 claims.
Because CVD remains the leading cause of death, the reality of undertaking CVD risk assessment via telemedicine needs to be considered. Currently, only clinic-measured blood pressure can be used for absolute CVD risk assessment. However, with the sustained use of telemedicine, alternative blood pressure measurement methods (eg home blood pressure) will be increasingly important for CVD prevention.20 Indeed, adding value to in-person presentations may be pivotal for the collection of CVD risk factor data. For example, referral to pathology services for lipid measurement is a key component for absolute CVD risk assessment and offers a setting to embed blood pressure measurement into existing care pathways. Previous work has demonstrated that blood pressure measurement can be undertaken at pathology services for absolute CVD risk assessment.21 In addition, an MBS item was recently introduced for ambulatory blood pressure monitoring, which could be undertaken via referral to pathology services.22
Strengths and limitations
A strength of this study is the use of nationally representative MBS data. However, the data were aggregate data and provide no information on what practices are using Item 699 or how the item is being used in practice. Further work with GPs to identify the factors driving uptake of Item 699 would be worthwhile to help inform best practice and identify opportunities to optimise uptake in primary care. We were unable to analyse characteristic-specific differences with the available data, but this could be explored in future work with alternative datasets. Finally, the authors acknowledge that specific MBS items do not reflect the complexity of patient care, and alternative funding models to support holistic care need to be considered in future health system changes.
Conclusion
This study of national MBS claims data demonstrates that uptake of Item 699 accounted for 9% of all health assessment item claims without a decline in pre-existing health assessment item claims. Item 699 had the greatest decline in health assessment item claims coinciding with the COVID-19 pandemic outbreak. With sustained adoption of telemedicine and blood pressure measurement as a key requirement to claim Item 699, these findings are important to consider how Item 699 can be delivered in a primary care environment with fewer in-person consultations.