Globally, hypertension causes more premature morbidity and mortality than any other risk factor.1 Uncontrolled blood pressure is a significant burden on Australia’s health, contributing to 43% of coronary heart disease, 38% of renal disease, 32% of atrial fibrillation and 3.6% of dementia.2 Blood pressure treatment and management are routinely offered in general practice, with hypertension accounting for 9.1 of every 100 general practitioner (GP) encounters.3 However, a clear evidence–practice gap exists4 because, despite the availability of evidence-based guidelines and effective pharmacotherapy,5 optimal blood pressure control remains elusive in up to 40% of Australians with known hypertension.6 This includes people at high absolute cardiovascular disease (CVD) risk, despite the evidence that this population derives the greatest cardiovascular risk reduction from blood pressure lowering.7 Despite the recognised benefits, evidence remains that many people with hypertension do not take the medications prescribed8 and/or still have lifestyle risk factors that could be reduced.9 Reducing these factors, by smoking cessation, enhanced nutrition, alcohol moderation and increasing physical activity, has the potential to reduce hypertension.5,9
There is an opportunity to enhance the care provided to people with uncontrolled blood pressure. Given their prolonged engagement and ongoing relationship with patients, nurses are ideally placed within the general practice team to work together with GPs to deliver interventions to improve blood pressure control.10 A recent systematic review of nurse-led interventions demonstrated improvements in blood pressure;11 however, evidence of the effectiveness of nurse intervention targeted towards people with hypertension and a high risk of CVD is limited due to a lack of robust trials in this area. The ImPress (Improving Blood Pressure Control in General Practice) intervention takes a novel approach in proactively directing nurse-led care to a high-risk population who have the most to gain from improved blood pressure control.12 This paper explores the characteristics of people living with hypertension and reports on a randomised pilot trial of the ImPress intervention on blood pressure outcomes.
Methods
The ImPress study was a pilot trial13 conducted between 2019 and 2021.This pilot trial used the same approach as the randomised controlled trial registered with the Australian and New Zealand Clinical Trials Registry (ID: ACTRN12618000169246)14 and was approved by the Human Research Ethics Committee of the University of Wollongong (Approval no. 2017/412). Due to the impacts of disaster and COVID-19,15,16 the sample size was smaller than the intended full trial.
General practices were approached by email, in addition to a wider recruitment strategy via local primary healthcare networks and nurse interest groups on social media. General practices that employed at least one registered nurse (general practice nurse [GPN]) and had computerised clinical systems were eligible to participate. Once enrolled in the study, the trial coordinator (CS) worked with GPNs to identify eligible patients at participating practices using clinical audit tools (eg Penn CS). Patients were eligible if they were regular patients of the practice (attended three or more times in the past two years), aged 45–74 years, diagnosed with hypertension, had a >15% risk of a CVD event in the next five years or pre-existing CVD17 and had blood pressure >140/90 mmHg at the assessment visit. Participants with insufficient electronic medical record data to calculate absolute cardiovascular risk or with no recorded blood lipids within the past five years were excluded. Due to financial constraints precluding translation, individuals were also excluded if their English comprehension impacted their ability to consent and participate in the study. Practices were randomised to intervention or control in blocks in a blinded manner by a statistician. The CONSORT guidelines18 were used to guide reporting.
Intervention
The ImPress intervention (Figure 1) was based on a previous pilot study.12 Intervention GPNs participated in a one-day workshop designed and delivered by GPN and medical experts. The content covered study procedures and data collection, including accurate blood pressure measurement, a blood pressure management protocol, motivational interviewing techniques and goal setting. Ongoing mentoring, telephone support and site visits were provided by the trial coordinator (CS).
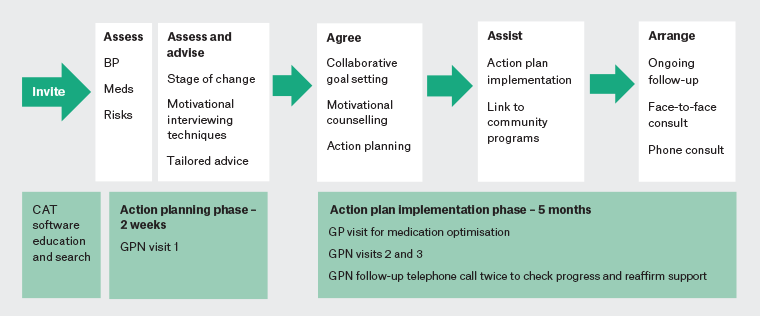
Figure 1. ImPress intervention. Click here to enlarge
BP, blood pressure; CAT, clinical audit tool; GP, general practitioner; GPN, general practice nurse;
ImPress, Improving Blood Pressure Control in General Practice; Meds, medications.
Over five months, intervention participants were offered five flexible nurse consultations delivered face to face or via telephone to improve blood pressure control and support lifestyle risk modification. GPNs worked in partnership with participants using the 5As framework19 to assess patients’ lifestyle risk, set goals for risk reduction and develop an action plan that detailed individualised lifestyle advice and agreed actions (Figure 1). As an example, the goal could be ‘to lose weight’, which was followed by an action plan based on lifestyle advise that focused on healthy eating (eg reduce salt, minimise carbohydrates and increase fruit and vegetable intake). GPs reviewed and optimised medications in line with current guidelines.5
The 2019–20 bushfires and the COVID-19 pandemic, which both occurred during the intervention phase of this study,16 had a significant impact on recruitment, retention and data collection.15 In some instances, face-to-face appointments were not possible, and telehealth was used to deliver the nurse visits. Blood pressure data were only included where data were collected in the general practice.
Control group GPNs received a three-hour training session that covered the same information as provided to intervention group GPNs regarding study recruitment, conducting medical record searches, data collection measures and accurate blood pressure measurement but no education on the ImPress intervention. Patients in the control arm received usual care during the study period.
Data collection
Participant demographic characteristics (Table 1), body mass index (BMI), medication adherence and lifestyle risk factors (smoking, nutrition, alcohol, physical activity [SNAP])19 were collected at baseline. Self-reported SNAP status was determined using questions from the Australian Bureau of Statistics Health Survey20 (Table 2). Because this was initially intended to be a full randomised controlled trial, the primary outcome was blood pressure, measured by GPNs using an automated office blood pressure device following National Heart Foundation guidelines.5 This was collected at baseline and six and 12 months.
| Table 1. Participant demographics |
| |
Intervention (n=30) |
Control (n=35) |
| n |
% |
n |
% |
| Sex |
| Female |
13 |
43.3 |
20 |
57.1 |
| Male |
17 |
56.7 |
14 |
42.9 |
| Age (years) |
| 45–54 |
4 |
16.7 |
4 |
12.5 |
| 55–64 |
6 |
25.0 |
7 |
21.9 |
| 65–74 |
14 |
58.3 |
21 |
65.6 |
| Education |
| Some high school |
9 |
36.0 |
3 |
8.8 |
| Completed high school |
3 |
12.0 |
8 |
23.5 |
| Vocational training |
4 |
16.0 |
9 |
26.5 |
| Tertiary education |
9 |
36.0 |
14 |
41.2 |
| Employment status |
| Working |
9 |
36 |
11 |
32.3 |
| Not currently working |
16 |
64 |
23 |
67.6 |
| Marital status |
| Currently married/de facto |
16 |
66.7 |
22 |
64.7 |
| Separated/divorced/widowed/never married |
8 |
33.4 |
12 |
35.2 |
| Born in Australia |
| Yes |
20 |
80.0 |
27 |
79.4 |
| No |
5 |
20.0 |
7 |
20.6 |
| SBP on eligibility screen |
| Grade 1 SBP 140–159 mmHg |
15 |
50.0 |
20 |
57.1 |
| Grade 2 SBP 160–179 mmHg |
13 |
43.3 |
9 |
25.7 |
| Grade 3 SBP >180 mmHg |
2 |
6.7 |
6 |
17.1 |
| SBP, systolic blood pressure. |
| Table 2. Baseline SNAP characteristics |
| |
Intervention |
Control |
Total |
| n |
% |
n |
% |
n |
% |
| Smoking |
| Non-smokers or former smokers |
20 |
66.7 |
26 |
74.3 |
46 |
70.8 |
| Currently smoke |
6 |
20.0 |
8 |
22.9 |
14 |
21.5 |
| Missing |
4 |
13.3 |
1 |
2.9 |
5 |
7.7 |
| Vegetable intakeA |
| Adequate daily intake |
4 |
13.3 |
13 |
37.1 |
17 |
26.2 |
| Inadequate daily intake |
21 |
70.0 |
21 |
60.0 |
42 |
64.6 |
| Missing |
5 |
16.7 |
1 |
2.9 |
6 |
9.2 |
| FruitA |
| Adequate daily intake |
4 |
13.3 |
2 |
5.7 |
6 |
9.2 |
| Inadequate daily intake |
18 |
60.0 |
32 |
91.4 |
50 |
76.9 |
| Missing |
8 |
26.7 |
1 |
2.9 |
9 |
13.8 |
| AlcoholB |
| Safe or no daily alcoholic consumption |
19 |
63.3 |
27 |
77.1 |
46 |
70.8 |
| Unsafe daily alcoholic consumption |
1 |
3.3 |
1 |
2.9 |
2 |
3.1 |
| Missing |
10 |
33.3 |
7 |
20.0 |
17 |
26.2 |
| Physical activityC |
| Adequate or high weekly physical activity |
3 |
10.0 |
9 |
25.7 |
12 |
18.5 |
| None or low weekly physical activity |
23 |
76.7 |
25 |
71.4 |
48 |
73.8 |
| Missing |
4 |
13.3 |
1 |
2.9 |
5 |
7.7 |
AAdequate intake is defined as five serves of vegetables and two serves of fruit daily.12
BSafe alcohol consumption is defined as no more than four alcoholic drinks on any day.12
CAdequate physical activity is defined as 75–100 min vigorous activity per week.5
SNAP, smoking, nutrition, alcohol, physical activity. |
Data analysis
Data were entered into SPSS (version 25; IBM Corp., Armonk, NY, USA) and checked for completeness and accuracy. Descriptive statistics were used to describe the demographic and SNAP characteristics of participants at baseline. Differences between systolic blood pressure (SBP) and diastolic blood pressure (DBP) were analysed at six and 12 months using a linear mixed model to adjust for clustering by practice. The random effect was the practice and the fixed independent effects were time and group. Analyses were not adjusted for multiple comparisons and the results should be interpreted in that light.
Results
Twelve general practices across South-Western Sydney and Southern Illawarra agreed to participate and were randomised by a statistician in a blinded manner. Of these 12 practices, 10 (five each in the intervention and control groups) completed the study (Figure 2). Of the 126 people screened, 55 (43.6%) were not eligible because their blood pressure was <140/90 mmHg at screening. Six (4.8%) eligible people declined to participate. Of the 65 eligible people recruited, 30 were from intervention group practices and 35 were from control group practices. The mean (±standard deviation [SD]) age of participants was 63.0±8.2 years in the intervention group and 66.0±8.2 years in the control group. Approximately half the intervention (50.0%) and control (57.1%) participants had grade 1 hypertension (SBP 140–159 mmHg) on eligibility screening (Table 1).
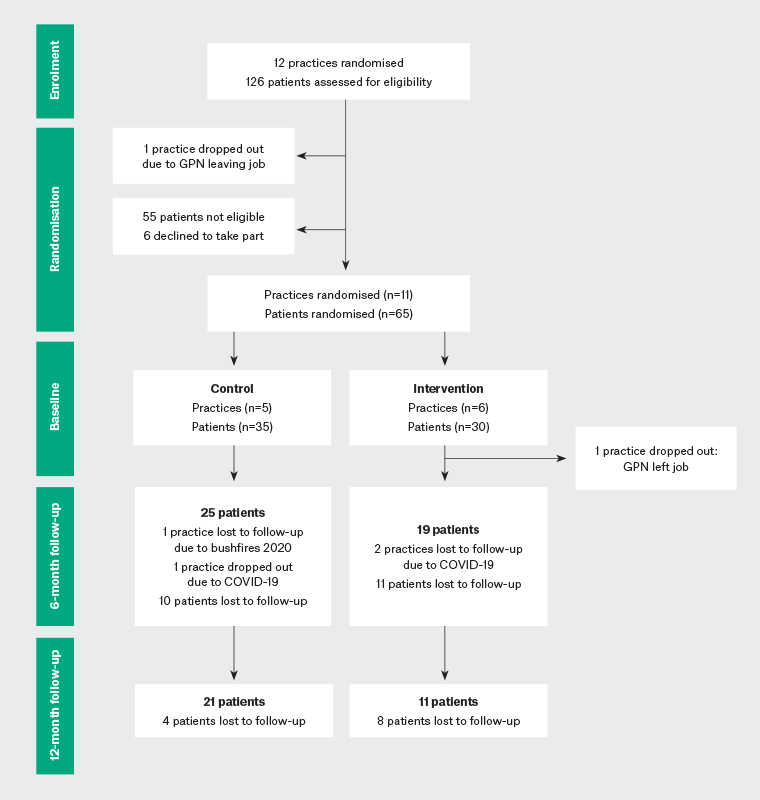
Figure 2. CONSORT flow diagram. Click here to enlarge
GPN, general practice nurse.
Lifestyle risk characteristics at baseline showed that most participants followed recommended guidelines concerning smoking and alcohol. However, fruit and vegetable intake and physical activity levels did not meet recommended levels in either group (Table 2).
At six months, the mean SBP in the intervention group had decreased by 25.1±23.3 mmHg from baseline (Table 3), and mean DBP had decreased by 10.6±14.3 mmHg from baseline. In the control group, mean SBP had also decreased, this time by 17.5±21.9 mmHg, and mean DBP had decreased by 8.9±13.3 mmHg from baseline. The adjusted mean difference between the groups at six months was 8.1 mmHg (95% confidence interval [CI]: –2.92, 18.94 mmHg; P=0.146) for SBP and 0.18 mmHg (95% CI: –6.54, 4.91 mmHg; P=0.775) for DBP. Neither of these differences was statistically significant.
| Table 3. Mean changes in systolic and diastolic blood pressure at 6 and 12 months |
| |
Systolic blood pressure (mmHg) |
Diastolic blood pressure (mmHg) |
| Baseline |
6 months |
MD in change |
12 months |
MD in
change |
Baseline |
6 months |
MD in change |
12 months |
MD in changeA |
| Control (n=25) |
161.4±16.2 |
145.4±19.1 |
17.5±21.9 |
152.0±15.1 |
7.7±12.0 |
90.8±15.5 |
81.8±10.0 |
8.9±13.3 |
87.7±23.3 |
0.5±27.2 |
| Intervention (n=19) |
159.7±13.4 |
138.5±15.9 |
25.1±23.3 |
140.0±17.9 |
18.9±15.9 |
90.8±12.0 |
83.8±11.4 |
10.6±14.3 |
80.6±13.5 |
7.5±11.6 |
| Adjusted MD (95% CI) between groups (mmHg) |
8.1 (–2.9, 18.9) |
11.3 (1.2, 21.4) |
0.18 (–6.5, 4.9) |
7.1 (–8.6, 22.9) |
| P-value |
0.146 |
0.030 |
0.775 |
0.362 |
Unless indicated otherwise, data are presented as the mean±standard deviation.
AMean difference (MD) in change was calculated for those with available outcome data.
CI, confidence interval. |
At 12 months, the mean SBP in the intervention group was 18.9±15.9 mmHg lower than baseline and mean DBP had fallen 7.5±11.6 mmHg from baseline (Table 3). In the control group, there was a 7.7±12.0 mmHg reduction in SBP and a 0.5±27.2 mmHg fall in DBP from baseline. There was a statistically significant between-group difference of 11.3 mmHg SBP at 12 months (P=0.03), but the difference in DBP of 7.1 mmHg was not significant (P=0.36).
Discussion
Although this became a pilot trial and the literature recommends that pilot studies should focus on process rather than outcomes, a previous review noted that it is common practice to report the outcomes of pilot research.21 Therefore, we have presented outcomes data to inform the calculation of effect sizes for future research and highlight the potential efficacy of the intervention. However, we acknowledge that given the pilot nature of this study, these data should be interpreted with caution.
The data revealed a substantial reduction in mean SBP from baseline to six and 12 months. The between-group SBP reduction found at six months was not as substantial as that reported in the previous pilot study (14.5 mmHg; 95% CI: –10.7, –18.2 mmHg).12 However, given that a decrease of just 5 mmHg SBP is associated with a 10% relative risk reduction of major cardiovascular events,5,22 this finding is clinically meaningful. A recent meta-analysis of GPN-led hypertension interventions found statistically significant reductions in mean SBP in trials with six-month or shorter follow-up with less pronounced effect in trials extending for 12 months or more.11 In contrast, our results show that a reduction in SBP was sustained, with participants maintaining improvement at 12 months. This highlights the potential for this kind of intervention to improve blood pressure control in the longer term and supports the need to conduct a larger-scale randomised controlled trial to provide robust effectiveness data. Further research is also required to elucidate the specific aspects of the intervention that contribute to this sustained effect. The reduction in DBP was also sustained at 12 months. The fact that this was not a statistically significant reduction was not surprising given that the mean DBP at baseline was only just above the normal threshold in both groups.
Baseline data in this study revealed valuable insight into lifestyle risk characteristics among people with hypertension and high CVD risk in general practice. Indeed, most participants did not meet recommended nutritional or physical activity guidelines.5 This is perhaps unsurprising given that only some 24% of Australian adults reportedly meet physical activity guidelines,23 and only one in 10 Australians meet the guidelines for daily vegetable intake.24 Despite the overwhelming evidence of the benefits of optimal nutrition and physical activity in managing blood pressure and preventing CVD,5,9 the continued high prevalence of these risk factors demonstrates that more can be done to support behaviour change in those most at risk. Further research is required to explore the sustainability of behaviour change in the risk factors identified.
Limitations
This trial set out to establish an evidence base for a GPN intervention to reduce hypertension. The study was planned as a sufficiently powered trial; however, the significant and unforeseen major bushfire and COVID-19 events greatly disrupted research and clinical activity, significantly impacting participant recruitment and retention and ongoing data collection.15 As a consequence, the planned sample size was not achieved. Therefore, we focused on the feasibility of the intervention and its potential effectiveness and have revised the findings to be viewed as a pilot trial. Achieving trial completion during this uniquely challenging time demonstrates researcher resilience and the dedicated effort of participating GPNs, GPs and consumers. It also demonstrates the feasibility of conducting a larger-scale trial and the potential for its effectiveness.
This study collected blood pressure as the primary outcome and originally planned to report secondary outcomes of lifestyle risk at six and 12 months. Due to the concurrent disaster and pandemic, insufficient follow-up data precluded this level of evaluation. Similarly, it was not feasible to collect data on general practice attendance among the control group. However, the baseline data provide important insights into the target population.
The analysis in this study is adjusted for clustering as per protocol; however, this should be interpreted with caution given the small sample size. Statistically significant data at 12 months could be due to participant bias because those who were more engaged with the intervention remained engaged in the study. In addition, the possibility of a type 2 error cannot be ruled out, meaning the intervention was effective. However, the sample size is small, resulting in the study not being sufficiently powered. Despite these limitations, the findings offer useful new insights into the potential of this intervention to improve health outcomes in this key area.
Conclusion
This pilot trial demonstrated that the ImPress intervention provided significant improvements in SBP that were sustained for 12 months. Although these data must be interpreted with caution, the pilot data support a growing evidence base that nurses can add value to the general practice team in the management of hypertension. Further investigation in the form of participating GPN, GP and patient feedback would help elucidate the successful elements of the intervention and provide insight into how the model could be effectively implemented in practice. These qualitative findings will be reported separately. The approach of active practice population management, where high-risk patients are identified and targeted for intervention, could also apply to other long-term health conditions. Further large-scale trials of the kind of team-based care advocated in this intervention are warranted.