Case
A woman aged 20 years presented with a more than three-month history of a scaly, erythematous rash to the groin. The rash was initially mild but had progressed and become persistent for approximately two months prior to presentation (Figure 1).
The rash was described as burning and uncomfortable. There was no history of atopy or psoriasis. The patient was otherwise well, except for a history of iron deficiency. She had seen a number of health practitioners and unsuccessfully trialled topical antifungals, topical corticosteroids and oral griseofulvin.
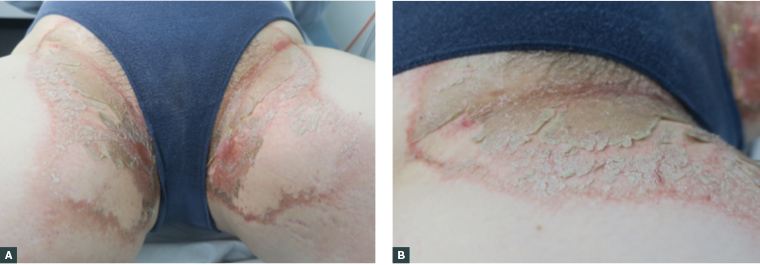
Figure 1A & B. A scaly and desquamating rash to the groin with a prominent erythematous margin
On examination, there was a bilateral intertriginous eruption affecting the groin creases with significant flaky desquamation and an erythematous margin. The changes extended into the lower abdomen, perineum and perianal areas.
A punch biopsy was taken, which demonstrated confluent parakeratosis and classical keratohyalin granules (Figure 2). No fungal hyphae were identified.
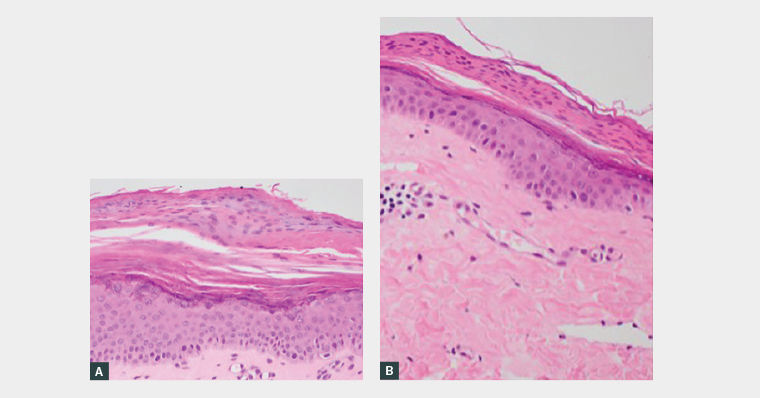
Figure 2A & B. A skin biopsy from the groin rash demonstrated histological findings consisting of confluent parakeratosis and acanthosis of the epidermis with retention of keratohyalin granules within the basal parakeratotic layer.
Question 1
What is the most likely diagnosis?
Question 2
What are other differentials to be considered?
Question 3
What causes this condition?
Question 4
What investigations should be done?
Question 5
How should this condition be managed?
Answer 1
This is a classical presentation of granular parakeratosis. Granular parakeratosis is a benign but distinct and distressing condition that typically affects intertriginous areas such as the axillae, groin or breast folds. The clinical appearance may include grouped, erythematous, scaly papules and plaques, and desquamation is usually a prominent feature. The condition may be unilateral or bilateral. The lesions are often initially asymptomatic, but may be associated with pruritus or burning discomfort.1 Granular parakeratosis can affect people of all ages and has no geographical or racial predilection. It is not associated with any systemic diseases.
Answer 2
There is a broad range of differentials to be considered in cases of granular parakeratosis, including conditions that classically affect the intertriginous zones or those that present with similar clinical findings.
The primary differentials to consider are atopic dermatitis, irritant or allergic contact dermatitis, flexural or pustular psoriasis, intertrigo, erythrasma, acanthosis nigricans, confluent and reticulated papillomatosis and hyperkeratotic napkin dermatitis.1 Acute generalised exanthematous pustulosis should be considered when there is an associated drug history, rapid onset and pustules. Less common but significant differentials to consider are extramammary Paget’s disease, Hailey–Hailey disease, pemphigus vegetans and Darier’s disease.1,2
It should be noted that granular parakeratosis has also been found concomitantly with other conditions, such as tinea corporis and bacterial impetiginisation.2
Answer 3
Granular parakeratosis is best described as an irritant contact reaction, although the exact pathogenesis is uncertain. Granular parakeratosis is often triggered by exposure to a number of topical agents, including zinc oxide, antiperspirants and benzalkonium chlorides (BACs), but may also arise without an identified trigger.3
There was no history of zinc oxide or antiperspirant use to the groin area in this patient, but it was revealed that her clothing was being washed using laundry products containing BACs.
BACs have antiseptic and preservative properties and are found in many common household items, including laundry rinses (Box 1).4 BACs are thought to act as surfactants, disrupting cellular lipid membranes and inactivating enzymes within the skin, inducing proliferation and causing abnormal development of keratinocytes.5 It has also been postulated that genetic susceptibility plays a role in the development of this reaction.6
| Box 1. Sources of benzalkonium chlorides3 |
- Household cleaning products, such as laundry rinses/detergents
- Personal care products
- Moisturisers, make-up removers, and cleansers
- Shampoos and hair products
- Wet wipes
- Antiseptics
- Eye drops and ophthalmic solutions, including:
- glaucoma treatments
- antibacterial eye drops
- corticosteroid eye drops
- antihistamine eye drops
- lubricating eye drops/artificial tears
- contact lens solutions
- Nasal sprays and asthma inhalers (tiotropium)
- Dental products
- Plaster of Paris
- Sterilisation solutions for medical instruments
- Industrial products used in:
- metallurgy
- agriculture
- fabrication of textiles and dyes
|
| Reproduced with permission of DermNet from Felmingham C, Nixon R. Benzalkonium chloride contact dermatitis. Hamilton, NZ: DermNet, 2019 (available at https://dermnetnz.org/topics/benzalkonium-chloride-contact-dermatitis). |
Answer 4
Granular parakeratosis is often diagnosed on clinical suspicion, but a skin biopsy may be completed for histopathological confirmation. Generally, histopathology reveals a characteristic appearance of a thickened stratum corneum with a distinctive granular appearance within the basal layer (Figure 2).7
Patch testing is usually not required because granular parakeratosis is an irritant mechanism as opposed to an allergic mechanism. Patients should only be referred for patch testing if there is a strong suspicion of allergic contact dermatitis. A skin swab for microscopy, sensitivity and culture should be completed if secondary bacterial or yeast infection is suspected. In addition, if tinea is suspected, then skin scrapings for fungal microscopy and culture may also be valuable.
Answer 5
First-line management is to remove any possible triggers that may have been identified on history. Once the specific contact factor has been withdrawn, the general trend is for slow self-resolution over time.
Aside from removal of the contact factor, there are no clear treatment regimens. Regular emollient and topical steroids may sometimes be of benefit, particularly if patients are symptomatic.1 More recently, success in resolving the rash has been reported with amoxicillin–clavulanic acid.8 Numerous other therapies have been trialled, but lack a robust evidence base (Table 1).1,8 If a concurrent bacterial or fungal infection is present, this should also be treated.
| Table 1. Potential therapies for granular parakeratosis1,8 |
| Topical |
Oral |
- Topical corticosteroids
- Antifungals
- Tretinoin
- Antimicrobial/antiseptic soaps
- Vitamin D analogues
- Topical calcineurin inhibitors
|
- Amoxicillin–clavulanic acid
- Corticosteroids
- Antifungals
- Isotretinoin
|
Case continued
Oral griseofulvin was ceased, and the patient was initially treated with emollient and topical methylprednisolone aceponate 0.1% ointment on the scaly and inflammatory border of the eruption, which was subsequently changed to a topical calcineurin inhibitor. Because of disease severity, she was also started on a course of amoxicillin–clavulanic acid.8
The patient was counselled to eliminate exposure to her BAC-containing laundry rinses, as well as other potential triggers. A review at six weeks (Figure 3) showed near-complete resolution, with some residual postinflammatory hyperpigmentation and increased prominence of the patient’s pre-existing striae.
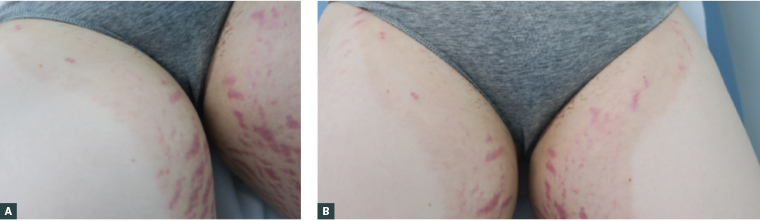
Figure 3A & B. Review at six weeks demonstrating near-complete resolution of granular parakeratosis. Note residual post-inflammatory hyperpigmentation changes and increased prominence of pre-existing striae.
Key points
- Granular parakeratosis is a benign but distinct condition that typically affects the intertriginous areas.
- Granular parakeratosis can be triggered by a number of common household chemicals, such as BACs, through the use of antiseptic laundry rinses and aids.
- The condition usually improves gradually over time after removal of the potential irritant and active treatment of the eruption.