Coronary heart disease is the leading cause of death in Australia, responsible for over 18,000 deaths in 2019.1 Yet atherosclerotic cardiovascular disease (CVD), including heart attacks, ischaemic strokes and peripheral vascular disease, is largely preventable, with modifiable risk factors accounting for up to 90% of the risk of a heart attack.2
Despite concerted implementation efforts in general practice, adherence to peak CVD prevention guidelines in Australia remains suboptimal.3 National guidelines have recommended regular cardiovascular screening for adults aged 45–74 years without a history of CVD since 2009.4 Yet one in three Australians eligible for absolute CVD risk assessment does not have up-to-date blood pressure and cholesterol measurements recorded in general practice software.5
‘Heart Health Check’ is a patient-friendly term for a comprehensive CVD risk assessment and ongoing management, subsidised through Medicare Benefits Schedule (MBS) Items 699 and 177 since April 2019. From April 2019 to April 2023, over 460,000 Heart Health Checks were delivered in general practice.6 In August 2019, Practice Incentives Program quality improvement (PIP QI) measures were introduced, including a measure on CVD risk.7 Data for the first year (2020–21) showed that over half of eligible patients still did not have sufficient data in their patient record to complete a CVD risk assessment.7
Barriers to Heart Health Checks remain, including a lack of access, time and awareness in the case of both general practitioners (GPs) and patients.8–10 Although opportunistic screening has been the mainstay of preventative CVD care for years, a more structured system for identifying at-risk patients and targeting screening activity is needed. With the national CVD prevention guidelines being revised in 2023, there is an urgent need to investigate new ways to overcome such barriers to improve implementation at scale. One option used in the UK is to recall target-age patients for a health check.11–13 Such programs are used for cancer screening in Australia,14–17 but they are managed via national registries rather than general practice, giving general practices limited control over their patient workload. Other countries have successfully used SMS recall systems for health checks that could be integrated into general practice software.11,18,19 The value of recall or reminder systems has also been shown in vaccination recall.20,21 There have been no structured SMS recall programs for CVD risk assessment in Australian general practice. Therefore, the aim of this study was to test the feasibility of a general practice–focused SMS recall system to invite eligible patients for a Heart Health Check.
Methods
Ethics approval
This study received ethics approval from the Royal Australian College of General Practitioners National Research and Evaluation Ethics Committee (NREEC 20-047).
Design
The feasibility study was based on a randomised design with two groups: an immediate intervention and a control group (the control group received access to the intervention after the study). General practices varied in size, location and rurality, and were randomised using a random number generator. Processes were documented, and a survey was sent to each intervention practice. General practices were eligible for the study if they were using CAT4 clinical audit software (Pen CS, Sydney, NSW, Australia), along with one of the following: BP Premier (Best Practice Software Pty Ltd, Bundaberg, Qld), Zedmed (Melbourne, Vic), Genie (Genie Solutions, Fortitude Valley, Qld), Medtech (Medtech Global, South Melbourne, Vic), practiX (Medical-Objects Pty Ltd, Maroochydore, Qld), Communicare (Telstra Health, Sydney, NSW), MMEx (ISA Healthcare Solutions, Bentley, WA) or PCIS (PCIS Gold, Provo, UT, USA). The analysis was blinded to randomisation allocation (analysis conducted using pseudocodes for group), but general practices that participated in the pilot could not be blinded to allocation.
Measures
Outcomes included general practice attendance in the past two months, updated CVD risk factors, Heart Health Check MBS item billing (Items 699, 177), Health Assessment MBS item billing (Items 701, 703, 705, 707 and 715, 224, 225, 226, 227 and 228) and general practice experience with the intervention. Data were recorded via clinical audit software (CAT4) and a general practice survey including questions about acceptability (eg staff time required to manage the intervention and patient response).
Recruitment
The study was advertised via existing general practice contacts, the Australian Practice Nurse Association, and primary health network organisations. In all, 332 general practices responded to the expression of interest, of which 231 eligible general practices were randomised (Figure 1).
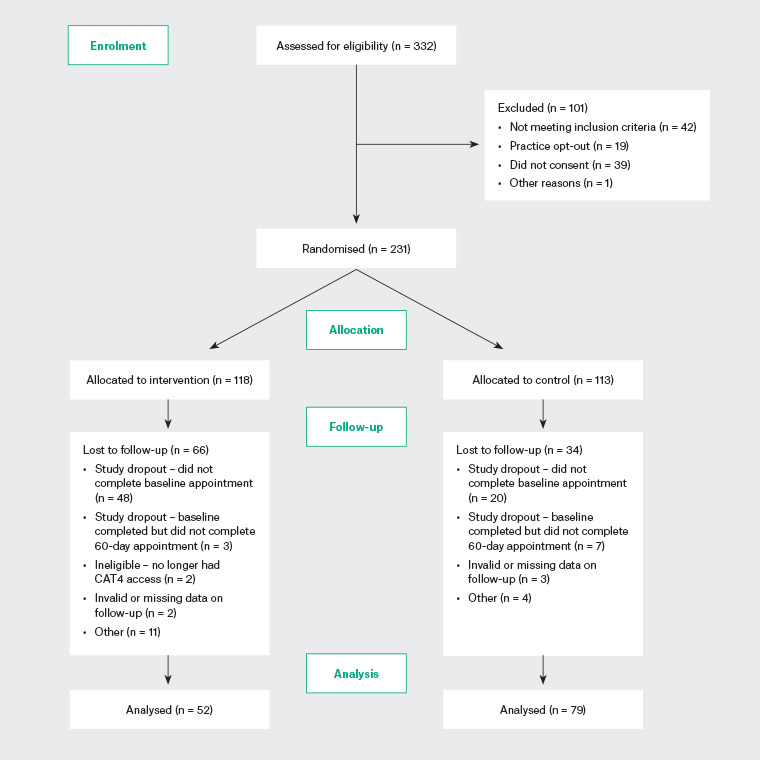
Figure 1. CONSORT diagram for general practice recruitment/retention. Click here to enlarge
Materials
Consumer testing of the SMS message and linked webpage was conducted by three authors. This included quantitative responses to alternative messages, and qualitative feedback from people with varying health literacy levels. The SMS and webpage text was edited to the recommended Grade 8 reading level to address health literacy needs. All authors discussed and agreed on the final message as a balance between a strong call to action and avoiding anxiety (see Appendix 1):
Hi [name], your doctor at [practice] would like to see you for a short Heart Health Check. Your age and other factors may raise your chance of a heart attack or stroke. Please call practice number to book. To learn more, visit landing page link. Reply STOP to opt out.
Intervention and process
At set-up, the embedded SMS recall feature (GoShare Plus) was enabled in the general practice’s clinical audit software (CAT4) and SMS credits were applied to each account. Costs for the SMS credits were covered by the Heart Foundation through a 12-month GoShare Plus licence for the Heart Health Check Recall bundle.
Guided by the study team over a telephone appointment, general practices in the intervention group used their clinical audit software to filter out a list of patients meeting the following eligibility criteria: age 45–74 years; no existing CVD; no health assessment or Heart Health Check in the past 12 months; total cholesterol and high-density lipoprotein cholesterol recorded in the past 12 months; and active patient (at least three visits in the past two years). General practices then used the embedded SMS feature to send the recall message to the list of eligible patients. The link included in the SMS redirected patients to a landing page with further information about the Heart Health Check, including patient testimonials, educational animations and awareness-raising tools. Although resources were provided to help general practice staff with booking and implementing Heart Health Checks, appointments that occurred as a result of the SMS recall were completed and billed as per the general practice’s usual billing procedures.
General practices in the control group continued their business as usual with no additional interventions. They received monthly email updates on the progress of the pilot and were given the option to send out recall messages after all data were collected for evaluation. General practices in both the intervention and control arms were provided access to information about the Heart Health Check, assessment and management templates and PIP QI resources via the Heart Foundation’s online Heart Health Check Toolkit .
Analysis
The program was funded to include up to 200 practices depending on interest and capacity during COVID-19. We anticipated the SMS intervention could create a 5% increase in screening and attendance based on similar published studies.11,13 Based on this assumption, 32 general practices (16 × 2 arms) would be required to detect a minimum difference of 5%. We over-recruited based on interest, assuming substantial dropout due to unpredictable COVID-19 burdens on general practice.
For variables with normal/Gaussian data distribution, data are reported as the mean and standard deviation. For variables with skewed distributions, data are reported as the median, and the 25% and 75% percentiles. A negative binomial regression was used. The suitability of the Poisson distribution was tested and the data were found to be over-dispersed, so a negative binomial was used. The dependent variable in the negative binomial regression was the count of Heart Health Checks observed during the two-month follow-up period. Models including billing policy and vaccination provider status were tested; however, the variables were not found to be statistically significant and they were excluded from the final model. General practice size (count of GPs) was excluded from the model due to collinearity with general practice volume (count of eligible patients). General practice volume was retained in the model because it was the more direct measure of the number of potential people eligible for a Heart Health Check. Interaction terms were tested for recall message and general practice volume/Socio-Economic Indexes for Areas (SEIFA) quintile, but neither was significant so they were excluded from the model. In all cases, two-sided P < 0.05 was considered significant.
Results
Pilot trial results
Practice characteristics
The CONSORT flow diagram is shown in Figure 1, and the baseline characteristics of the general practices in the two groups are presented in Table 1. Characteristics were similar between the control and intervention groups. Drop-out was greater in the intervention than control group (66 vs 34, respectively), but the characteristics remained balanced between arms. The final analysis included 79 practices in the control arm and 52 in the intervention arm.
| Table 1. Baseline practice characteristics |
| |
Control practice (n = 79) |
Intervention
practice (n = 52) |
P-value |
| Median (25%, 75% percentile) no. eligible individuals per practice |
554 (257–807) |
509.5 (316–836) |
0.597A |
| Median (25%, 75% percentile) no. eligible individuals contactable per practice |
503 (232–776) |
498 (303–789) |
0.566A |
| Practice size (%) |
| Solo (1 GP) |
6.3 |
3.8 |
0.563B |
| Small (2–5 GPs) |
55.7 |
59.6 |
| Medium (6–10 GPs) |
27.8 |
32.7 |
| Large (≥11 GPs) |
10.1 |
3.8 |
| Practice volumeC (%) |
| Small (≤500 patients) |
48.1 |
48.1 |
0. 998D |
| Medium (501 to ≤1000 patients) |
34.2 |
34.6 |
| Large (>1000 patients) |
17.7 |
17.3 |
| Rurality (%) |
| Major cities of Australia |
65.8 |
47.1 |
0.083D |
| Inner regional Australia |
24.1 |
37.3 |
| Outer regional/remote Australia |
10.1 |
15.7 |
| SEIFA quintile (%) |
| 1 (most disadvantaged) |
12.7 |
25 |
0.236D |
| 2 |
22.8 |
9.6 |
| 3 |
24.1 |
25 |
| 4 |
20.3 |
21.2 |
| 5 (least disadvantaged) |
20.3 |
19.2 |
| Billing policy (%) |
| Full private billing |
8.9 |
5.8 |
0.429B |
| Fully bulk-billed |
39.2 |
30.8 |
| Mixed |
51.9 |
63.5 |
| Providing COVID-19 vaccinations at baseline (%) |
| No |
16.5 |
21.6 |
0.6156D |
| Yes |
83.5 |
78.4 |
| Month of baseline evaluation (%) |
| April |
38.0 |
29.4 |
0.3738B |
| May |
49.4 |
51.0 |
| June |
6.3 |
15.7 |
| July |
5.1 |
1.9 |
| August |
1.3 |
1.9 |
AWilcoxon rank-sum test.
BFisher’s exact test.
CPractice volume is based on the number of eligible patients at baseline.
DChi-squared test.
GPs, general practitioners; SEIFA, Socio-Economic Indexes for Areas. |
In the intervention arm, 41,586 eligible participants received a recall SMS; of these, 13.2% (n = 5486) clicked on the embedded web link for more information.
Outcomes
Outcomes and analyses are presented in Tables 2 and 3. The median number of eligible individuals attending general practices in the two months after the recall message was sent did not differ significantly between intervention and control practices (410 vs 411, respectively; Table 2). However, there was a statistically significant increase in intervention practices in the number of Heart Health Checks (MBS Items 699 and 177; median 67.5 vs 0) and health checks in those aged 45–49 years (median 2 vs 1) compared with control practices (Table 2). Looking at the number of ‘75+’ (MBS Items 701, 703, 705, 707, 715, 224, 225, 226, 227 and 228) and ‘other’ health assessments, there were no differences between the two arms. (‘Other’ health assessments are described as health assessments for Aboriginal and Torres Strait Islander peoples aged 15–54 years, Aboriginal and Torres Strait Islander peoples aged 55+, people with an intellectual disability, residents of aged care facilities, refugees and other humanitarian entrants, and type 2 diabetes evaluation for people aged 40–49 years with a high risk of developing type 2 diabetes.) The additional Heart Health Checks in the intervention group were not replacing other health checks. Figure 2 shows the relationship between the number of eligible individuals receiving a Heart Health Check at two months and the number of eligible individuals. There is a pattern of increasing Heart Health Checks with an increasing number of eligible patients, with substantial separation between the control and intervention practices.
| Table 2. Outcomes by randomised group |
| Outcome |
Control practice
(n = 79) |
Intervention practice (n = 52) |
P-value |
| No. eligible individuals attending in the two months after baseline |
411 (185–272) |
410 (272–657) |
0.681A |
| Ratio of eligible individuals at two months:eligible individual at baseline |
0.81 (0.20)B |
0.83 (0.20)B |
0.650C |
| No. eligible individuals receiving a Heart Health Check (Items 699 or 177 billed) in the two months after baseline |
0 (0–5.5) |
67.5 (37–95) |
<0.001A |
| Ratio of eligible individuals receiving a Heart Health Check (Items 699 or 177 billed) within two months:eligible individuals at baseline |
0.01 (0.03)B |
0.15 (0.10)B |
<0.001B |
| No. eligible individuals receiving a 45- to 49-year health check in the two months after baseline |
1 (0–3) |
2 (0–6) |
0.022A |
| No. eligible individuals receiving a 75+ health check in the two months after baseline |
11 (5–29) |
11.5 (4–31) |
0.970A |
| No. eligible individuals receiving other health checks in the two months after baseline |
0 (0–2) |
1 (0–2) |
0.307A |
Unless indicated otherwise, data are given as the median (25th–75th percentile).
AWilcoxon rank-sum test.
BMean (SD).
Ct-test. |
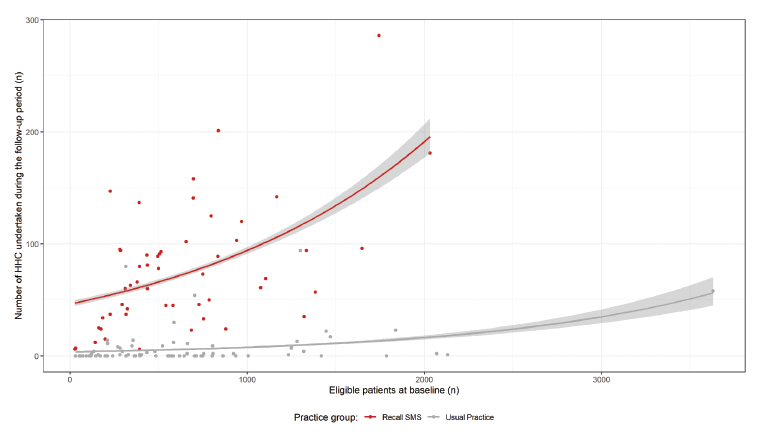 Figure 2. Number of eligible patients receiving HHCs at two months plotted against the number of eligible patients at baseline in intervention (recall SMS) and control (usual practice) general practices. Click here to enlarge
Figure 2. Number of eligible patients receiving HHCs at two months plotted against the number of eligible patients at baseline in intervention (recall SMS) and control (usual practice) general practices. Click here to enlarge
HHC, Heart Health Check.
Regression models
The results of negative binomial generalised linear regression models are presented in Table 3. This analysis indicates a strong association between sending a recall SMS and increasing Heart Health Checks in the following two months. After controlling for other variables (practice size, rurality and SEIFA), a general practice that sends a recall SMS to eligible patients is expected to have approximately 14-fold (incidence rate ratio = 13.9) more Heart Health Checks in the following two months compared with a similar general practice that did not send recall messages. More Heart Health Checks were associated with outer regional/remote regions, larger general practices (>1000 eligible patients at baseline) and less disadvantaged areas (SEIFA Quintile 3 > Quintiles 1–2).
| Table 3. Regression models for Heart Health Check billing data |
| |
IRR |
95% CI |
P-value |
| Recall message (reference = no recall) |
| Recall message sent |
13.9 |
7.2, 27.5 |
<0.001 |
| Practice volume (reference = medium) |
| Small |
0.9 |
0.4, 1.7 |
0.670 |
| Large |
2.4 |
1.0, 6.0 |
0.0454 |
| Rurality (reference = major cities) |
| Inner regional Australia |
1.5 |
0.7, 3.4 |
0.290 |
| Outer regional/remote Australia |
2.8 |
1.1, 8.0 |
0.047 |
| SEIFA quintile (reference = 3) |
| 1 (most disadvantaged) |
0.3 |
0.1, 0.9 |
0.016 |
| 2 |
0.3 |
0.1, 0.8 |
0.001 |
| 4 |
0.6 |
0.3, 1.6 |
0.349 |
| 5 (least disadvantaged) |
0.9 |
0.4, 2.3 |
0.842 |
| CI, confidence interval; IRR, incidence rate ratio; SEIFA, Socio-Economic Indexes for Areas. |
Process evaluation
Participant characteristics
Survey consent was obtained from a subsample of 35 intervention practices, of which 19 general practices responded (54% response rate). This included 53% regional, 42% metropolitan and 5% remote general practices, with practice managers being most likely to respond on behalf of the general practice (63%).
Quantitative survey questions
Most general practices had previously used health recall systems (90%), including SMS (63%). The intervention was acceptable to participants overall, with all respondents indicating the recall pilot was ‘somewhat’ (26%) or ‘very’ (74%) effective, and all interested in continuing to use the recall process (100%). The average likelihood of recommending the recall system to other general practices was rated 8.8 out of 10. The use and usefulness of each intervention component is reported in Appendix 2. Most practices (84%) held briefing sessions prior to sending the SMS, and the most commonly used resources were information for practice staff (74%) and the Heart Health Check Toolkit (68%), both of which were rated as ‘very’ or ‘somewhat’ useful by over 90% of respondents.
In terms of patient response to the SMS, the most common response was to call the practice to schedule a Heart Health Check (reported by 100% of respondents) or request more information (74%), visiting the practice to schedule a check (37%) or to obtain more information (21%), and making an online booking (21%). The response was most commonly perceived to be the same day as the SMS (47%) or in the same week (32%).
Qualitative feedback in open responses
Open responses indicated a pivotal role for practice managers and practice nurses in managing the intervention as champions:
It was a team effort but practice manager and practice nurse thought out the steps and lead it.
The briefing session was perceived as useful for ensuring the whole practice team was ready for the intervention:
They were ready for the patients calling.
Reminder for GPs about the different billing options – either 699 or as part of standard attendance.
Preparing for the patient response to SMS in advance was particularly important during periods of high demand for other appointments, like vaccination:
Probably sending less messages at a time as the phone lines were extremely busy and then due to COVID vaccination clinics we had limited [appointment] times.
The patient response to SMS was seen as positive and useful as a repeated strategy:
The phone went crazy directly after the SMS messages went out – patients were excited about being called in about their heart health and wanted to book in as soon as possible. I would have loved to be able to send a second batch two months after the first one, to get those that we couldn’t accommodate.
Overall, the intervention had positive feedback as a useful way to engage patients in Heart Health Checks, as long as this was done during periods where the amount of appointments could be managed. Different models were used by different practices, generally involving reception staff to manage calls and appointments, and both a nurse and GP to conduct the checks:
We had 30 minutes booked in with health nurse then follow on appointment with [the patient’s] GP, to finalise the check. We did 3 days a week 8 am to 5 pm. Most days it was fully booked (back-to-back appointments). We were fully booked for 3 months! A huge success.
We made one appointment with nurse being 15 minutes and doctor being 15 minutes. Had to book one to two months after message was sent out due to current bookings. Reception staff did a great job themselves in working out how to describe and explain Heart Health Check.
Discussion
Principal findings
To our knowledge, this is the largest targeted cardiovascular screening trial of its kind in Australian general practice. This feasibility study shows that an SMS recall intervention for CVD risk assessment can be acceptable to Australian general practices in both metropolitan and rural areas, even during periods with a high burden on general practice staff during COVID-19. We found preliminary evidence that targeted recall SMS can increase Heart Health Check delivery 14-fold, and our data suggest that this was not simply a diversion of general health checks to a different MBS item but a real increase in screening. The process evaluation indicated good acceptance of the program and highlighted the importance of good preparation before the rollout of such an intervention, including the need to manage a large amount of calls in the first day and week after the SMS is sent. Practice managers and practice nurses were seen as pivotal champions of the intervention; reception staff were involved in managing the response and providing more information; and nurses and GPs required coordinated appointment times to manage the Heart Health Checks. The practices used various models to manage this process, including staggered SMS sends over several weeks, booking out certain days for back-to-back Heart Health Checks and organising preconsultation tests if required. Importantly, the intervention needed to be planned by individual practices around other priorities.
Comparison to prior work
Previous Australian trials have had some success in increasing CVD risk assessment in general practice, including waiting room preconsultation22 and clinical decision support.23,24 However, their effect has been limited to a small number of trial general practices and required specific resources that do not necessarily fit within business-as-usual processes. This study demonstrates the feasibility of a scalable intervention, because mobile phone use is very high in Australia25 and other countries have successfully rolled out national SMS-based screening programs.11,13 The release of new CVD prevention guidelines planned for 2023 provides an opportunity to implement a targeted national screening program.
Future directions
Our team has used these pilot findings to run a more complex implementation trial (underway over 2022–23) aiming to replicate these results in higher-risk areas and with patients who have less recent engagement in their preventative cardiac health (Australian New Zealand Clinical Trial Registry ID: ACTRN12622000140752). We also plan to test the effect of a nudge (reminder) SMS and different messages that use various behaviour change strategies to increase interest and uptake, based on findings from cancer screening programs in Australia and the NHS health check program in the UK.11,13 Our findings also have implications for letter-based cancer screening programs in Australia. Understanding the link between attendance after recall and cardiovascular risk factor management and subsequent outcomes would be an area of interest for future studies. Future research could investigate why there was a strong negative correlation between socioeconomic disadvantage and Heart Health Check billing after recall.
Strengths and limitations
The main strength of this feasibility study is its large sample despite COVID-19 disruptions, its wide geographical reach and the demonstration of an intervention process that is acceptable in both regional and metropolitan areas. The intervention was largely delivered by general practice staff under real-world conditions, leveraging existing practice workflows. This helps improve the generalisability of the results to Australian general practices.
Limitations include COVID-19 disruptions, which led to uneven dropout rates between the intervention and control groups, although baseline characteristics remained balanced. This intervention was delivered while COVID-19 vaccinations were being delivered in primary care. It is possible that busier general practices were more likely to withdraw from the intervention arm due to concerns around capacity issues, but, at the time, this could not be measured. It is also possible that the practices that withdrew, assuming withdrawals were COVID-19 related, do not reflect ‘usual practice’ outside of the pandemic. Because practices responded to recruitment advertisements to participate, volunteer bias may be present.
The process evaluation survey was only conducted in a small number of participating general practices, so may overestimate acceptability.
Conclusion
This study showed that an SMS recall program for Heart Health Checks can be effective and acceptable in Australian general practice. Future research will confirm these findings with a broader trial targeting high-risk regions and patients, with reinforced messaging strategies.