Over the last decade in Australia, the burden of disease for children experiencing non-acute conditions, such as behavioural, developmental and some mental health issues, has been increasing.1,2 This is evidenced by more frequent presentations of children in mental health crises to hospital emergency departments and by long outpatient waiting lists for assessment of behavioural or developmental concerns, which has been exacerbated by the COVID-19 pandemic.3–5 General practitioners (GPs), who are doctors qualified in general medical practice, are often the first point of contact for someone with a health concern. In the Australian primary care setting, GPs are at the forefront of child and adolescent healthcare6,7 and play a crucial role in addressing the growing disease burden in this age group.8,9 Preparation of trainee doctors (referred to as GP registrars) for this key role begins during specialist training in general practice.
The amount of exposure to non-acute paediatric presentations that GP registrars receive during training might impact their confidence when managing these conditions, where confidence refers to a belief in their abilities at carrying out a particular skill or knowledge set.10 A UK survey of paediatric registrars reported that over half felt inadequately prepared for managing long-term, chronic conditions, as their training was primarily in acute care settings.11 GP registrars were expected to be even less confident than paediatric registrars as they receive less exposure to non-acute paediatrics during their GP training.11
The Registrars Clinical Encounters in Training (ReCEnT)12 study documents the in-consultation clinical and educational experiences and actions of GP registrars across Australia. Data from this study indicate that paediatric encounters during GP training are mostly for acute presentations. Further, GP registrars typically seek more advice from their supervisors and make referrals more often for paediatric patients than for adult patients.6,13 One explanation for these findings is that GP registrars experience a relative lack of confidence in treating non-acute paediatric presentations. Our recent study of Victorian GP registrars found that prevocational paediatrics training was mainly obtained in acute care settings and that registrars lacked confidence in managing non-acute biopsychosocial conditions compared to acute medical conditions (such as infections, acute asthma).14
At the time of the present study, most Australian GP registrars obtained their Fellowship in general practice via the Australian General Practice Training (AGPT) program, delivered by nine broadly state-based Regional Training Organisations (RTOs). Within this program, registrars could follow one of two training paths: the Royal Australian College of General Practitioners (RACGP) Fellowship pathway15 or the Australian College of Rural and Remote Medicine (ACRRM) Fellowship pathway16 (Figure 1). The RACGP three-year training pathway17 requires registrars to accrue experience with paediatric patients prior to commencing supervised vocational clinical training in a general practice clinic.18 This paediatric experience is predominantly in acute care settings19 (RACGP guidelines for paediatric encounters focus solely on emergency presentations, with no reference to non-acute conditions19), with a smaller number in community settings. Some registrars also elect to complete additional paediatric training through theory-based coursework via the Diploma of Child Health (DCH) (recently renamed to the Sydney Child Health Program). The ACRRM training pathway includes the completion of one of five paediatric training options at any time during the four-year program.16 From February 2023, delivery of GP training in Australia transitioned from RTOs to a centralised training program under the RACGP or ACRRM. One-to-one, on-the-job training provided by an appointed clinical GP supervisor remains unchanged.20
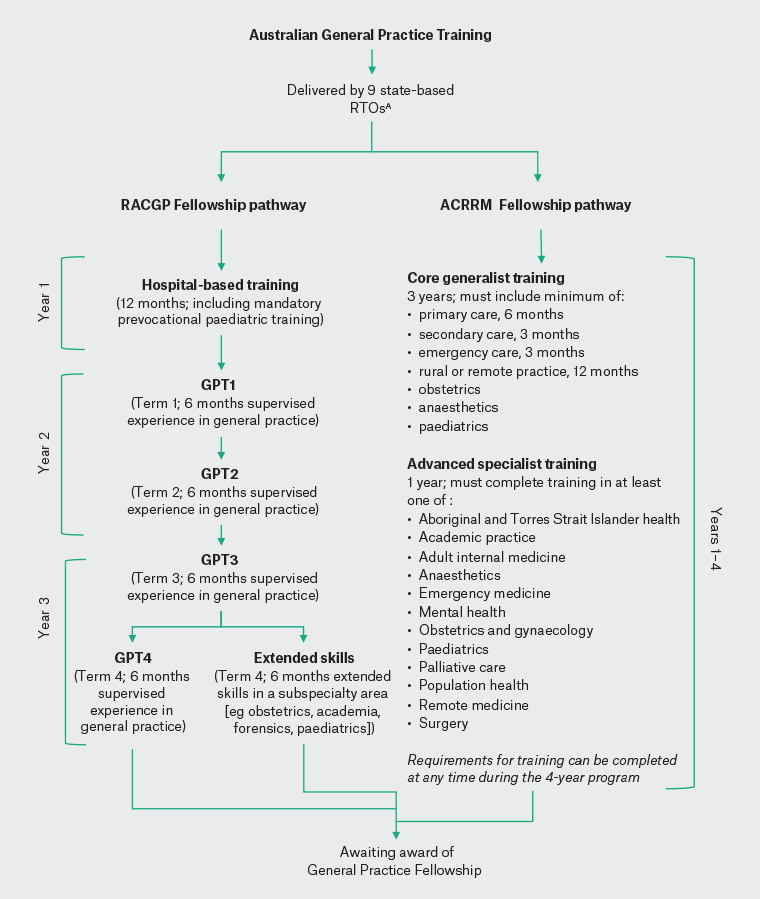
Figure 1. Australian General Practice Training pathways. Click here to enlarge
AAt the time of data collection.
ACRRM, Australian College of Rural and Remote Medicine; GPT, general practice training; RACGP, The Royal Australian College of General Practitioners; RTOs, Regional Training Organisations.
Given the differences in paediatric training for GP registrars between the RACGP and ACRRM pathways, the present study set out to examine in a national sample whether GP registrar confidence varied according to training experiences. Specifically, the key aims of this study were to examine differences in GP registrars’ levels of confidence in managing paediatric presentations in primary care by training pathway, RTO, training level, DCH experience, presentation type (acute/non-acute/routine immunisations) and prevocational paediatric experiences. In addition, differences in confidence managing paediatric and adult patients were assessed to examine whether variation in confidence was specific to consultations with children or apparent across consultations with a variety of age groups and presentations.
Methods
A consortium of advisors and chief investigators was formed for this study, which included representatives from the RACGP (R McCoy) and ACRRM (RI), along with each Australian RTO (including NS, LM, PM, MB and CB) and researchers from primary care (CM, IW, LS) and paediatric health services (HH).
Study design, setting and participant recruitment
All GP registrars enrolled in an AGPT program (RACGP or ACRRM) between September and October 2019 were eligible to participate in this cross-sectional study. Those still completing hospital-based prevocational training or not enrolled in the AGPT program were ineligible.
Two approaches were available to RTOs to recruit participants according to their preference, both capturing anonymised responses (Box 1). Prior to survey launch, the study was advertised in RTO newsletters, Facebook pages and bulletin boards. Participants were invited via email to complete an online survey using the Qualtrics XM survey platform (Qualtrics, Provo, UT, USA).
| Box 1. Study recruitment methods used by Regional Training Organisations |
Method 1: Regional Training Organisation (RTO) made initial email contact with all their registrars and offered an option of opt-out from further contact. Those not opting out received a follow-up email with a unique survey ID enabling reminder emails to be sent only to those who had not completed the survey. The following participating RTOs used this recruitment method:
- General Practice Training Tasmania (GPTT, Tas)
- Western Australian General Practice Education and Training (WAGPET, WA)
- General Practice Training Queensland (GPTQ, Qld)
- Northern Territory General Practice Education (NTGPE, NT)
Method 2: RTO made initial email contact with all their registrars using a generic survey link, rendering survey responses anonymous; a pre-set number of reminder emails was sent to all registrars regardless of whether they had completed the survey. The following participating RTOs used this recruitment method:
- GPSynergy (NSW and ACT)
- James Cook University (JCU) GP Training (Qld)
- GPEx (SA)
- Metro City Country Coast (MCCC, Vic)
- Eastern Victoria General Practice Training (EVGPT, Vic)
|
Data collection
The online survey, based on our previous Victorian study,14 included questions on demographics, training pathway (RACGP/ACRRM), training term (General Practice Training [GPT] 1–4/extended skills or awaiting fellowship) and types of paediatric prevocational experiences.
Participants’ overall confidence in managing paediatric presentations and their confidence managing different clinical presentations (eg acute, non-acute and routine care [ie immunisation]) were assessed using five-point Likert scales (very low confidence [1] to very confident [5]). Confidence in managing similar presentations in adult populations was also captured as a point of comparison. The survey was piloted with seven GP registrars and early career GPs prior to launch.
Data analysis
Descriptive statistics were generated for participant demographic characteristics and confidence levels. To address the key aims, three analyses were undertaken. First, unadjusted and confounder-adjusted ordinal regression models were fitted to examine differences in overall confidence in managing primary care paediatrics and each of the training pathways, RTO, training level and DCH experience (analysis #1). Second, for RACGP registrars only, confidence was assessed by prevocational paediatric experiences (analysis #2). Prevocational paediatric experiences were collapsed into three mutually exclusive categories reflecting increasing exposure to paediatric-specific experiences: (i) general population (ie those whose paediatric rotations were solely in emergency medicine in a general hospital with mixed paediatric and adult patients); (ii) exclusive paediatric (ie those whose paediatric rotations were either in a paediatric hospital or solely seeing paediatric patients in a general hospital); and (iii) exclusive paediatric plus additional specialist training (ie those seeing only paediatric patients and also undertaking additional paediatric training and/or community-based paediatric health experiences). Finally, descriptive statistics and regression models were examined for associations between presentation type (acute/non-acute/routine) and patient age group (adult/paediatric) and confidence (analysis #3).
All analyses were performed using Stata/IC 16 (StataCorp, College Station, TX, USA). Ethics approval was granted by the Human Research Ethics Committee of the University of Melbourne (ethics ID# 1953789.3). Authors had full access to all the data (including statistical reports and tables) in the study.
Results
Demographics and response rate
Of 3554 eligible GP registrars, 977 (28%) commenced the survey; of these, 894 (92%) provided complete data for analysis one (Appendix 1). Response rates by RTO are provided in Appendix 2.
Most participants (93.2%) were enrolled in the RACGP training pathway, were female (67.8%) and in the age range of 25–35 years (71.9%). The demographic profile of GP registrars taking part in the study was broadly representative of the overall population of Australian GP registrars,13 with comparable proportions by training pathway (RACGP versus ACRRM) and RTO, but with a greater proportion of females in the study sample (Table 1). Further, the proportion of GP registrars who participated from each RTO was broadly reflective of the distribution of registrars across the country.
| Table 1. Demographic and training characteristics of participating GP registrars (n=894) compared to AGPT population characteristics (n=4008) |
| |
Study sample
(n=894) |
AGPT populationA
(n=4008) |
| |
n |
(%) |
n |
(%) |
| Gender |
| Male |
288 |
(32.2) |
1751 |
(40.7) |
| Female |
606 |
(67.8) |
2552 |
(59.3) |
| Age (years)B |
| 25–30 |
344 |
(38.5) |
/ |
|
| 31–35 |
299 |
(33.4) |
/ |
|
| 36–40 |
136 |
(15.2) |
/ |
|
| 41–45 |
56 |
(6.3) |
/ |
|
| 46+ |
59 |
(6.6) |
/ |
|
| Training pathwayC |
| RACGP |
833 |
(93.2) |
4011 |
(93.3) |
| ACRRM |
61 |
(6.8) |
292 |
(6.8) |
| Regional Training Organisation (Australian state)D |
| GPSynergy (NSW/ACT) |
200 |
(22.4) |
1387 |
(32.1) |
| GPTQ (Qld) |
136 |
(15.2) |
582 |
(13.5) |
| JCUGPT (Qld) |
41 |
(4.6) |
466 |
(10.8) |
| NTGPE (NT) |
30 |
(3.4) |
111 |
(2.6) |
| WAGPET (WA) |
154 |
(17.2) |
453 |
(10.5) |
| GPEx (SA) |
87 |
(9.7) |
352 |
(8.2) |
| GPTT (Tas) |
33 |
(3.7) |
113 |
(2.6) |
| EVGPT (Vic) |
109 |
(12.2) |
356 |
(8.3) |
| MCCC (Vic) |
104 |
(11.6) |
488 |
(11.3) |
| Training levelB |
| GPT1 |
126 |
(14.1) |
/ |
|
| GPT2 |
332 |
(37.1) |
/ |
|
| GPT3 |
144 |
(16.1) |
/ |
|
| GPT4/Extended skills |
260 |
(29.1) |
/ |
|
| Awaiting Fellowship |
32 |
(3.6) |
/ |
|
| DCH enrolmentB |
| Yes |
330 |
(36.9) |
/ |
|
| No |
564 |
(63.1) |
/ |
|
AData drawn from the AGPT 2019 National GP registrar survey conducted by ACER.17
BValues not available for the AGPT population, indicated by /.
CValues for the RACGP training pathway combine all dual training options: FRACGP and FRACRRM; FRACGP and FARGP; FRACGP, FARGP and FACRRM.
DSee Box 1 for Regional Training Organisation definitions.
AGPT, Australian General Practice Training; ACRRM, Australian College of Rural and Remote Medicine; DCH, Diploma of Child Health; FACRRM, Fellowship of the Australian College of Rural and Remote Medicine; FARGP, Fellowship in Advanced Rural General Practice; FRACGP, Fellowship of the Royal Australian College of General Practitioners; GP, general practitioner; GPT, general practice training; RACGP, Royal Australian College of General Practitioners. |
Overall confidence managing paediatric presentations
Almost three-quarters of GP registrars reported feeling confident (confident = 65.3%; very confident = 8.3%) in managing paediatric presentations (Figure 2A), with very few participants reporting low confidence (very low or low confidence combined = 3.3%). Confidence levels were found to vary little by training pathway (Figure 2B), but were higher for those in more advanced training levels (Figure 2C) and those with DCH experience (Figure 2D). Regression modelling results showed strong evidence of higher confidence with increasing training term, even after adjusting for effects of covariates including age (adjusted OR=12.3, 95% CI=5.2–29.1, P<0.001 comparing those awaiting fellowship to those in GPT1) and among those with DCH experience (adjusted OR=2.0, 95% CI=1.5–2.8, P<0.001; Appendix 3).
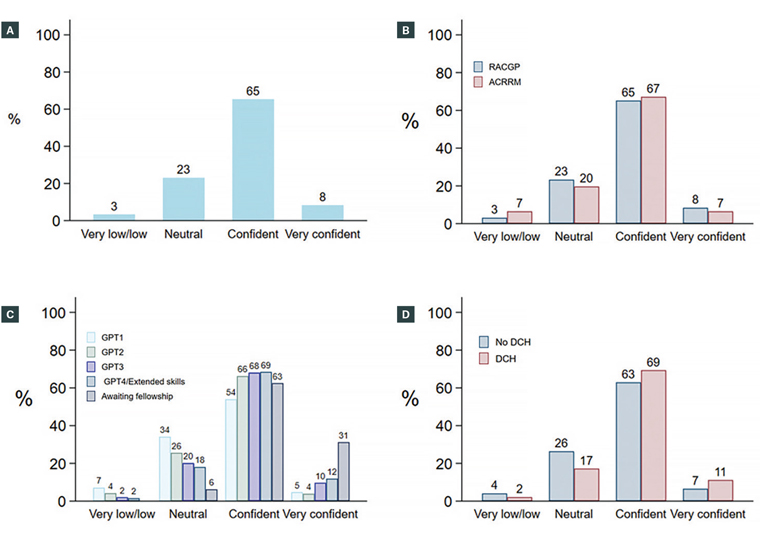
Figure 2. Overall confidence in managing paediatrics for: (A) the entire sample and by (B) training pathway, (C) training level and (D) Diploma of Child Health (DCH) experience. Click here to enlarge
ACRRM, Australian College of Rural and Remote Medicine; GPT, general practice training; RACGP, The Royal Australian College of General Practitioners.
Overall confidence managing paediatric patients by type of paediatric prevocational training experience was examined among a subset of GP registrars (n=770) who provided these data (Figure 3). The highest overall reported confidence was from GP registrars whose prevocational experiences included exclusive paediatric patient experience (ie either in a paediatric hospital or only seeing paediatric patients in a general hospital) and additional specialist training (eg DCH and/or community paediatric experience), with 85% reporting feeling confident or very confident. This was followed by those with exclusive paediatric patient experience (71%). Those with prevocational experiences only in emergency medicine in a general hospital (ie combining mixed paediatric and adult patients from the general population) had the lowest percentage reporting feeling confident or very confident (56%). There was strong evidence of a difference in confidence by prevocational training experience supporting these descriptive findings (eg adjusted OR=6.74, 95% CI=4.0–11.4, P<0.001 comparing those with exclusive paediatric plus DCH or community experience to the general population; Appendix 3).
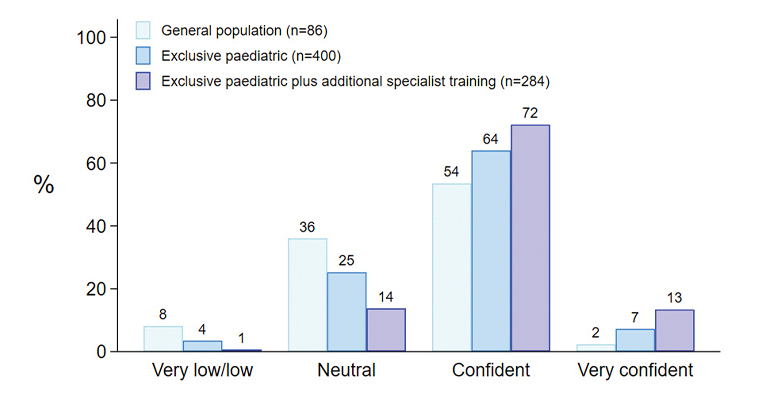
Figure 3. Overall confidence in managing paediatrics by type of paediatric prevocational training experience.A
AData from a subset of participants who provided data on different paediatric prevocational experiences (n=770).
Confidence managing acute and non‑acute paediatric presentations
Results show clear differences in confidence managing acute and non-acute paediatric presentation types (Figure 4). The percentage reporting confident or very confident was much higher when managing acute presentations, such as upper respiratory tract infections and asthma (74–95%) than when dealing with non-acute paediatric presentations, such as mental health, autism and soiling (13–46%). These descriptive findings were supported by strong evidence from regression models of a difference in confidence by presentation type (eg adjusted OR=41.4, 95% CI=37.2–46.1, P<0.001 comparing management of acute presentations with non-acute presentations; Appendix 4).
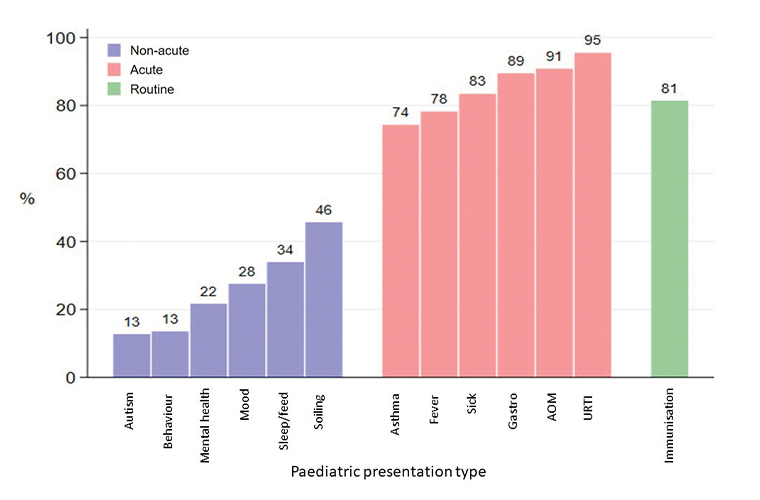
Figure 4. Proportion reporting confident or very confident in managing paediatric patients by paediatric presentation type (colour coded according to presentation grouping: blue=non-acute; red=acute; green=routine immunisation).
Key: Behaviour, behavioural problems; Mood, mood disorders; Sleep/feed, sleeping and feeding issues; Fever, febrile illness; Sick, recognition of the sick child; Gastro, gastroenteritis; AOM, acute otitis media; URTI, upper respiratory tract infection.
Finally, we compared GP registrars’ confidence with paediatric patients (being treating both for acute and non-acute conditions) versus their confidence with adult patients encountering these same conditions. Overall, GP registrars were less confident working with paediatric compared with adult patients. Registrars were also less confident when managing non-acute versus acute conditions in both adult and paediatric patients (Figure 5). Results of regression modelling showed evidence of higher confidence when working with adult patients compared with paediatric patients both for non-acute presentations (adjusted OR=3.12, 95% CI=2.9–3.4, P<0.001) and acute presentations (adjusted OR=3.94, 95% CI=3.5–4.4, P<0.001; Appendix 4).
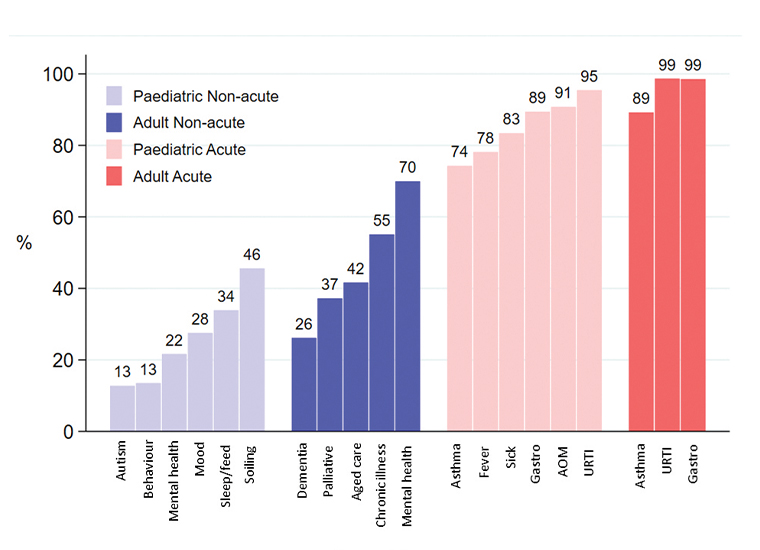
Figure 5. Proportion reporting confident or very confident in managing presentation by adult or paediatric presentation type (colour-coded according to presentation grouping: purple=non-acute paediatric; blue, non-acute adult; pink, acute paediatric; red, acute adult.
Key: Behaviour, behavioural problems; Mood, mood disorders; Palliative, palliative care; Fever, febrile illness; Sick, recognition of the sick child; Gastro, gastroenteritis; AOM, acute otitis media; URTI, upper respiratory tract infection.
Discussion
Findings show that overall confidence levels among GP registrars in managing primary care paediatric patients in Australia are higher for those who completed prevocational training experiences with a paediatric focus compared with those whose prevocational experiences were more generalist (ie focused on the general population in emergency departments only). Importantly, this study also found that GP registrars are less confident managing non-acute paediatric presentations in the primary care setting as opposed to acute presentations – even though many children present to GPs with non-acute presentations.20
This finding might be explained, at least in part, by recent Australian data showing that prevocational paediatric training experiences typically occur in the acute setting;19 that is, prominence of these types of paediatric encounters during GP training might contribute to the overall comparative confidence in acute paediatric consultations, as opposed to non-acute paediatric conditions.
These findings suggest we should be looking at novel ways to introduce more community-based and other non-acute paediatric care experiences to increase GP registrar confidence prior to vocational training, especially given the increasing burden these issues are causing Australian children.2
In contrast to indirect indicators of reduced GP registrar paediatric confidence (such as increased referral rates and increased assistance from supervisors for paediatric patients from the ReCEnT study6,18), our study directly examined registrar confidence at all training levels and found it lacking in non-acute paediatric care. This highlights a possibility for guided clinical training experiences in non-acute paediatrics to be offered as a way to enhance GP registrar confidence. One example of such a program is the Melbourne-based ‘Strengthening Care for Children’ program, which embeds paediatricians into GP clinics for co-consultation, case discussion and advice in a bid to reduce referral rates and ED presentations for non-acute conditions. This program resulted in increased GP confidence when managing these and other paediatric conditions.20
Strengths and limitations
A key strength of this study is recruitment across the entire national cohort of Australian GP registrars due to collaboration with all nine of Australia’s state-based RTOs at the time. The response rate of 28% is comparable to other GP and GP registrar online surveys.21 Although the possibility of non-response bias and consequent impacts to generalisability are acknowledged for moderate response rates, we sought to mitigate these risks by establishing that our study sample was broadly representative of the national population of Australian GP registrars, with a small exception for gender.
Limitations include inability to include GP registrars in the ACRRM stream in analyses examining associations between prevocational experience and confidence. They were excluded as their paediatric experience occurs during and not prior to entering clinical general practice settings. Further, this study focused on self-reported GP registrar confidence in managing paediatric consultations (ie a belief in their abilities at carrying out a particular skill or knowledge set22) and not competence (ie being technically proficient in putting these abilities into practice22). Research suggests these two constructs are poorly correlated.22,23 Although it was beyond the scope of the present study, future work might further explore the relationship between GP registrar confidence and competence in primary care paediatrics.
Conclusion
The finding that GP registrars have lower confidence in non-acute paediatrics is concerning given the increasing demand on Australian GPs to identify and manage paediatric non-acute problems, which have trebled in number for GP consultations over 12 years.7 This, together with rising presentations of mental health conditions to paediatric emergency departments3 and other chronic issues managed in already stretched hospital outpatient clinics due to the COVID-19 pandemic, creates an urgent need to reform GP registrar training in non-acute paediatrics. Solutions could include targeted GP educational strategies in non-acute paediatric clinical consultations, as well as increasing the availability of paediatric prevocational experience by accrediting paediatric outpatient clinics, private paediatrician rooms or primary care practices with paediatric expertise. The recent transition from RTOs to the RACGP and ACRRM for the responsibility of training GP registrars creates an ideal opportunity to address this training deficit through the new centralised program.