If we had a pill that conferred the proven health benefits of exercise, doctors would prescribe it to every patient and healthcare systems would find a way to make sure every patient has access to this wonder drug.
– Dr Bob Sallis, founder of the
Exercise is Medicine Initiative
Most Australian adults (approximately 85%) are insufficiently physically active based on the current national physical activity guidelines.1 Physical inactivity is a major contributor to the development of several chronic diseases, including poor mental health, arthritis, type 2 diabetes, cardiovascular disease, cancer and chronic obstructive pulmonary disease.2 Sustained population-level approaches to increase physical activity are required to drastically reduce this disease burden.
In general practice, approximately 1.5 per 100 encounters involve a discussion about physical activity.3 Only 1.44 per 1000 consultations involve a referral to an accredited exercise physiologist (AEP) and only approximately 5% of referred consultations under the enhanced primary care Chronic Disease Management (CDM) scheme are for AEPs.4 During the COVID-19 pandemic, individuals with lower cardiorespiratory fitness levels experienced worse COVID-19 severity and hospitalisation outcomes,5,6 and physical inactivity levels were associated with poorer mental health outcomes.7 Now, there is opportunity to prioritise exercise care in general practice for all individuals with chronic disease who are more likely to experience ill health from COVID-19 and who are likely to benefit the most from increasing physical activity. The aim of this paper is to provide an overview of exercise care approaches to support patients living with chronic disease who are looking to sustainably increase physical activity levels. In doing so, we have provided a brief overview of the importance of physical activity promotion and exercise care for people living with chronic conditions; collated resources to support the assessment and prescription of exercise in general practice; and provided an overview of emerging approaches to exercise that are garnering evidence to support their use at the population level for sustained increases in physical activity.
Physical activity is a human right
The World Health Organization (WHO) emphasises the importance of physical activity and its accessibility to all individuals, with a global call to action to achieve a ‘paradigm shift in both supporting and valuing all people being regularly active, according to ability and across the lifecourse’.8 The 2012 Lancet series on physical activity declared physical inactivity a worldwide pandemic due to its substantial health impact and economic, environmental and social consequences.9 The sustainability of exercise is intricately linked with broader definitions of sustainability for global wellness, with a specific lens on equity.10 The United Nations’ 2030 Agenda for Sustainable Development includes a specific goal to ‘ensure healthy lives and promote well-being for all at all ages’ (Goal 3), with a subgoal (3.4.1) to reduce non-communicable disease mortality rates, including those associated with cardiovascular disease, cancer, diabetes and chronic respiratory disease, through prevention and treatment.11 In the context of physical activity, this extends to safe environments and access to affordable and quality exercise services and professionals, which requires scaled and global awareness and investment.8
Exercise as a ‘vital sign’
‘Exercise’ refers to planned and structured physical activity for the purpose of health, wellness and/or performance maintenance or gain. Arguably, the most important outcome of regular exercise is the improvement in cardiorespiratory fitness. Cardiorespiratory fitness, which is measured by the maximum rate of oxygen consumption (VO2max), reflects the integrated system capacity for oxygen transport, uptake and utilisation. Low cardiorespiratory fitness is one of the strongest prognostic markers for cardiovascular disease and all-cause mortality in people with chronic disease,12 and is the strongest predictor of healthcare costs in people with coronary artery disease.13 Given their potency for risk prediction, physical activity/exercise and cardiorespiratory fitness should be considered as clinical vital signs in clinical practice.14 In general practice, exercise screening tools and non-exercise fitness tests can be readily used to estimate these clinical outcomes (see ‘Assess’ below; Table 1).
| Table 1. Resources |
| |
Resource description |
Link |
| Ask and assess |
Exercise is Medicine Australia’s Physical activity stage of change: Assessment tool |
https://exerciseismedicine.org.au/resources/tools-forms/ |
| RACGP’s Healthy habits – patient pathways, clinical dashboard and resource hub for lifestyle behaviour change |
https://healthyhabits.racgp.org.au/ |
| World Fitness Level – evidence-based non-exercise fitness tests to estimate cardiorespiratory fitness |
www.worldfitnesslevel.org/#/
|
| Advise and assist |
Handbook of non-drug interventions (HANDI) – for physical activity-related fact sheets and ‘how-to’ guides for a broad range of chronic conditions |
www.racgp.org.au/clinical-resources/clinical-guidelines/handi |
| ESSA – position and consensus statements supporting practical translation of research into practice for a broad range of chronic diseases |
www.essa.org.au/Public/Advocacy/Position_Statements.aspx |
| TGROW coaching model infographic from TPC Health for key components of effective health coaching conversations |
https://tpchealth.com/wp-content/uploads/2020/06/Structuring-a-Health-Coaching-conversation-TPC-Health.pdf |
| Exercise is Medicine Australia’s fact sheets: ‘Professional’ (for doctors, nurses and allied health professionals) and ‘Public’ (for patients and the general public) on exercise for the prevention, treatment and management of chronic conditions or disorders |
https://exerciseismedicine.org.au/resources/factsheets/ |
| GoShare for health-related text messaging support and handouts that can be embedded in practice |
https://westvicphn.com.au/health-professionals/health-topics/digital-health/goshare/ |
| Active Ageing Australia for physical activity promotion and support across the lifespan – active ageing information, programs, training and resources |
https://activeageing.org.au/ |
| Arrange |
Exercise is Medicine Australia’s exercise prescription and referral form |
https://exerciseismedicine.org.au/resources/tools-forms/ |
| Find an ESSA-accredited exercise professional |
www.essa.org.au/find-aep/ |
| Parkrun and the RACGP parkrun practice initiative to promote the health and wellbeing of staff and patients |
www.parkrun.com.au/
RACGP - parkrun practice |
| Heart Foundation Walking to find a walking group or community for a specific area |
https://walking.heartfoundation.org.au/walking |
| Live Life Get Active nationwide not-for-profit social prescription initiative |
https://livelifegetactive.com/social-prescribing-article/ |
| Australian Government – physical activity and exercise resources |
www.health.gov.au/topics/physical-activity-and-exercise/physical-activity-and-exercise-resources |
| Ask and (re)assess |
Free fitness and activity tracking applications |
www.strava.com/
www.myfitnesspal.com/
www.apple.com/au/ios/health/
https://developer.android.com/guide/health-and-fitness/health-connect |
| RACGP Healthy Habits – mobile application to track patient progress |
https://healthyhabits.racgp.org.au/ |
| ESSA, Exercise and Sports Science Australia; RACGP, The Royal Australian College of General Practitioners; TGROW, Topic, Goal, Reality, Options, Will. |
What is impacting exercise sustainability?
Clinicians play an essential role in raising the topic of exercise in consultations and advocating for its role in the prevention and management of chronic disease. Clinicians are viewed as trusted authorities for health information; however, physical activity is rarely assessed or discussed during clinical visits.15 Advice alone is typically insufficient for behaviour change, as evidenced by research on weight loss.16 Furthermore, according to the UK’s National Institute for Health and Care Excellence (NICE), for every 14 inactive individuals who receive brief advice on physical activity, only one person will report an increase in their physical activity levels.17 Nevertheless, general practitioners (GPs) are well placed to deliver behaviour change interventions, and often patients are receptive to behaviour change interventions from their GP.18 From a patient perspective, barriers and enablers to the uptake and maintenance of exercise are multifactorial, with broad biopsychosocial factors underpinning individual participation (Figure 1).19,20
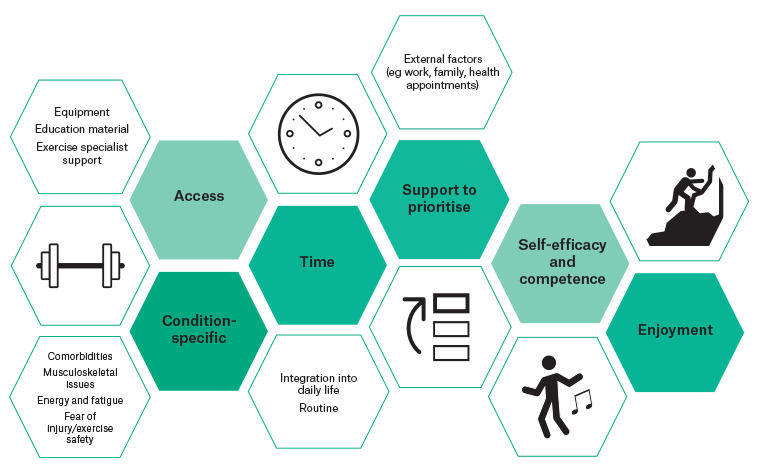
Figure 1. Factors underpinning the uptake and maintenance of exercise in people living with chronic disease. Click here to enlarge
Sustainable solutions for patients living with chronic disease
Every patient should receive an assessment of their current physical activity levels at least annually, as well as a prescription and referral to qualified professionals, supports or resources for further counselling and monitoring.
The GP action plan: Primary care consultation
An interdisciplinary approach to exercise care has been recommended for GPs, whereby physical activity behaviour change is prioritised, assessed and prescribed by GPs, with tailored support including referral to AEPs for individualised exercise assessment and prescription and/or to community support where appropriate.21,22 A GP action plan should be guided by the 5As of behavioural counselling (Assess, Advise, Agree, Assist, Arrange), with a framework for time considerations outlined in Figure 2.
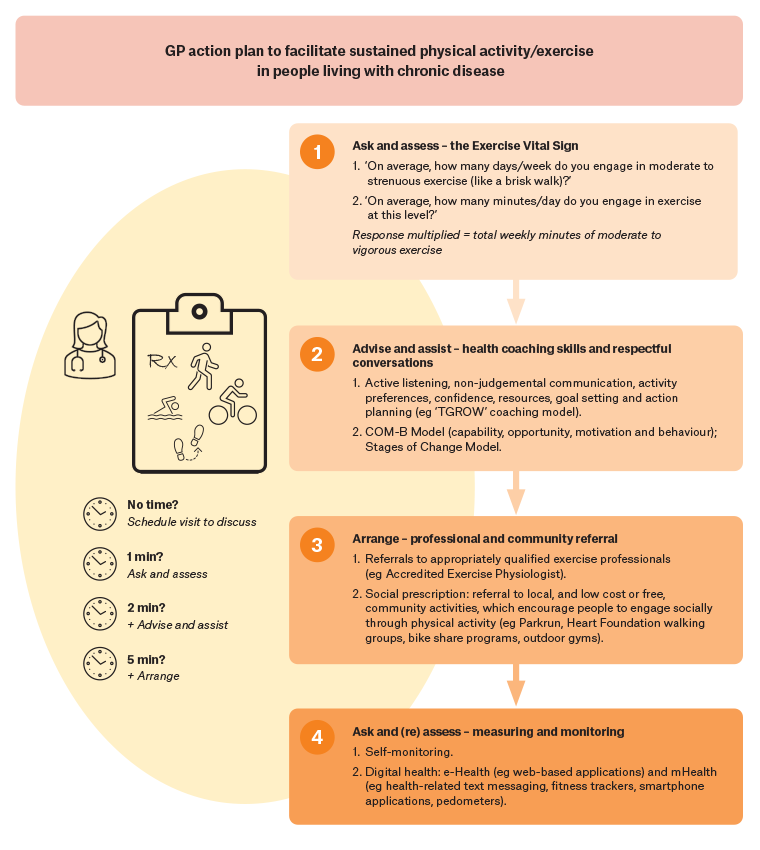
Figure 2. A framework for general practitioner (GP) action to facilitate sustained physical activity and exercise in people living with chronic disease. Click here to enlarge
Assess
Several tools have been developed to facilitate physical activity screening within general practice.23 The Exercise Vital Sign takes less than 30 seconds to administer and can be used to identify people who are inactive and in need of physical activity counselling and support (Figure 2). A feasible and practical tool to estimate cardiorespiratory fitness is via a validated non-exercise fitness test;24 for example, via the World Fitness Level website (Table 1). Patient responses should be recorded in medical software to enable monitoring and reassessment (eg in Best Practice or Medical Director, under ‘recreational activities’).
Advise and assist: Health coaching skills and respectful conversations
Brief targeted conversations that focus on physical activity education and goals can be effective at promoting behaviour change.25 Underpinning conversations with health coaching theory and techniques can enable clinicians to adopt a person-centred approach and assists individuals to articulate their health goals and develop the necessary knowledge, skills and confidence to self-manage their health. Health coaching conversations draw on health behaviour change theories to frame conversations and build self-efficacy (Figure 2).26,27 These approaches encourage people to identify what is meaningful for them and act on their intentions enabling lasting behaviour change for improved wellbeing; the ‘best’ exercise prescription is one that an individual will enjoy and continue long term. There are several resources supporting GPs with appropriate exercise recommendations. Over 15 exercise-specific clinical practice guides are available through The Royal Australian College of General Practitioners’ (RACGP) Handbook of non-drug interventions, such as exercise for type 2 diabetes, depression and chronic fatigue syndrome (Table 1). Detailed information on nuanced modification of exercise programming for a broad range of chronic conditions endorsed by professional bodies is also available (Table 1).
Arrange: Professional and community referral
Although the promotion, assessment and prescription of exercise begin at the general practice consultation, professional and community referral can optimise the health service to provide tailored patient management. Referral to an AEP might be facilitated under CDM for eligible patients (Table 1). In a recent study, people living with non-alcoholic steatohepatitis and obesity expressed that exercise professional support was a highly valued enabler of exercise adherence.20 With the support of an AEP, participants completed 12 weeks of supervised high-intensity interval training (HIIT) with excellent adherence to the high-intensity heart rates and physical exertional targets, number of intervals and session attendance, despite multiple comorbidities, musculoskeletal injuries and polypharmacy.28 However, once the exercise professional support was removed, exercise was not sustained.20
Social prescribing is another approach rapidly gaining popularity worldwide as a means for enabling people to overcome social determinants of health associated with physical inactivity.29 Social prescribing encourages healthcare workers to connect people to community-based services and activities to improve holistic health and wellbeing.30 Alternatively, a referral to a ‘social prescribing link worker’, where available, provides opportunities for a more in-depth discussion and facilitated connection to local sources of community support. In fact, the RACGP parkrun practice initiative has been designed to support GPs to socially prescribe to local parkrun events (Table 1).
Ask and (re)assess: Measuring and monitoring
Self-monitoring progress can support people to make sustained behaviour changes. Digital health technologies are revolutionising healthcare across primary, secondary and tertiary sectors,31 and might have an increasingly larger role in supporting chronic disease prevention in healthcare.32 Over 90% of Australians have a smartphone and the use of wearable technologies increased steadily from 28% of adults in 2020 to 58% in 2021.33 e-Health interventions, such as web-based applications and software programs, are becoming more common in exercise care for chronic conditions.34 Often these programs allow users to access predetermined exercise routines, track dietary intake and exercise sessions and connect with other users. Recent evidence has shown that e-Health exercise interventions are safe, feasible and enjoyable for patients with chronic disease35,36 and have clinical use in improving various health markers.37–39
Mobile health (mHealth) involves the use of mobile devices to provide exercise care.34 Wearable devices linked with mobile applications often use unique features (such as step counting and behavioural movement ‘nudges’) to help provide monitoring and accountability and can be effective for improving fitness, body composition and physical activity.40 In Australia, GoShare is a common platform that can be embedded in clinical practice to provide text-messaging support and handouts following a consultation. Prior practice with technology, gradual scaling of administrative coaching, appropriate workforce training and empowerment of consumers to choose digital health solutions to healthcare might facilitate use.41 Overall, digital health approaches to exercise care might be useful as a sustainable option for patients to engage with to increase physical activity levels.
Exercise ‘dosing’: How low can we go?
Modest increases in physical activity duration are exceptionally important, especially when a low-active individual goes from doing nothing to doing something regarding physical activity. With perceived lack of time being one of the most cited barriers to exercise, a stepped approach to exercise is recommended for those who are inactive (ie focusing on small, sustained increases in daily physical activity with progression towards physical activity guidelines). Indeed, the Australian Institute of Health and Welfare reports that if the nine in 10 individuals who were ‘at risk’ of chronic disease added just 15 minutes of daily moderate intensity exercise, it could potentially avoid 13% of future physical inactivity-related disease burden; increasing this to 30 minutes would double this health saving.2 This is a particularly important consideration for people living with chronic disease who are more likely to have low baseline exercise capacity and low cardiorespiratory fitness; that is, encourage individuals to progressively develop exercise-related self-efficacy and progress as exercise capacity increases. Regarding exercise composition, as per principles of exercise programming, structured exercise should involve a warm-up, tailored aerobic and/or resistance exercise training and a cool-down. People living with chronic diseases might require a longer cool-down period (5–10 minutes) to prevent postexercise hypotension. Although there is ample evidence to support the promotion of 150–300 minutes per week of moderate–vigorous physical activity, several approaches to exercise that seek to overcome common barriers to sustainability have been proposed.
Is it a ‘HIIT’?
To address ‘lack of time’ as a barrier to physical activity, there has been considerable interest in the utility of HIIT to improve health and fitness. HIIT involves one or more bouts of high-intensity exercise interspersed with lower-intensity recovery periods. There is a substantial body of literature supporting the safety, efficacy and feasibility of HIIT in people with chronic disease when appropriately screened, supervised and monitored.28,42 Indeed, even low-volume HIIT (Figure 3) has been shown to improve cardiorespiratory fitness, cardiac function, blood glucose control and blood pressure.43 However, despite clinical benefits and apparent safety and feasibility in supervised, screened settings, no study to date has been able to demonstrate long-term adherence to self-directed HIIT.44 This is likely due to challenges implementing HIIT beyond a highly supervised and resource-heavy laboratory or clinical environment (eg research settings or cardiac rehabilitation settings where HIIT is increasingly used); thus, without additional support, HIIT might not be a sustainable exercise solution at a population level. Moreover, clinical guidelines for the safe delivery of HIIT in chronic disease emphasise that medical screening, cardiopulmonary evaluation, modest exercise progression and continued monitoring of patient health and medication status are necessary.45 High-intensity training might be contraindicated in some people with chronic disease, and it is noteworthy that physical activity is heath promoting regardless of intensity. GPs can assist by overseeing the medical guidance, continuing to encourage physical activity where clinically safe or arranging clinically safe physical activity, which might include referral to an AEP.
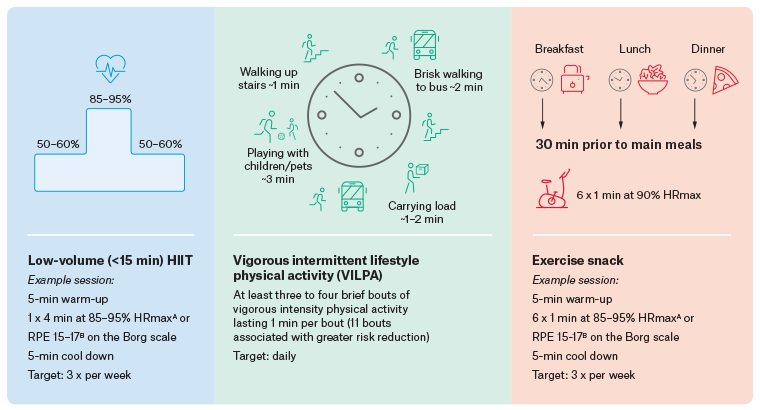
Figure 3. Novel, potentially sustainable exercise solutions for people with chronic disease. Click here to enlarge
AMaximum heart rate (HRmax) is calculated as (208 – [0.7 × age]) for adults not on medication affecting heart rate (eg beta-blockers). BRating of perceived exertion (RPE) from the Borg 6–20 scale, where 15 is ‘hard’ and 17 is ‘very hard’.
HIIT, high-intensity interval training.
Vigorous intermittent lifestyle physical activity
Emerging research suggests that incorporating three to four short bouts of vigorous intermittent lifestyle physical activity (VILPA) each day might significantly reduce mortality rates.46 VILPA includes brief bursts of vigorous physical activity; for example, power walking, running for the bus or taking flights of stairs (Figure 3). A study using data from the UK Biobank and published in Nature Medicine observed an up to 40% reduction in all-cause and cancer-related mortality and an approximate 50% reduction in cardiovascular disease-related mortality in individuals who engaged in VILPA.46 Importantly, approximately 90% of the 25,000 non-exercising participants in the study engaged in some level of VILPA, making it a feasible and potentially effective early target for sustainable physical activity. However, it is worth noting that larger volumes of VILPA were associated with greater benefits. For example, engaging in 11 bouts of VILPA each day was associated with a 65% reduction in cardiovascular disease-related mortality and a 49% reduction in cancer-related death than doing no VILPA each day. These findings were comparable to the 62,000 UK Biobank participants who undertook structured vigorous-intensity exercise, suggesting that the manner by which vigorous bouts of activity were accrued (ie purposefully or incidentally) was less important than the total accumulation of VILPA.46
Exercise snacks
Exercise snacks have been proposed as a novel strategy to improve cardiometabolic health.47 Exercise snacks are brief periods of vigorous physical activity generally lasting approximately one to five minutes that aim to accumulate small, frequent doses of moderate–vigorous physical activity throughout the day (Figure 3). Unlike VILPA, exercise snacks are not purely incidental; they can be planned, targeted and potentially timed to fit within a daily schedule, at the home or office. Emerging evidence suggests that exercise snacks might be particularly beneficial for glycaemic control when timed around meals. Francois et al showed that six one-minute bouts of high-intensity exercise three times daily before main meals led to improved glycaemic control (reduction of 24-hour mean glucose concentration by an average of 0.7 mmol/L, which persisted for 24 hours) in people with insulin resistance.48 A clinically meaningful improvement in cardiorespiratory fitness (ie 1 metabolic equivalent) was observed following a six-week stair-climbing protocol (3×20-second hard effort over a 10-minute period) on just three days per week.49
Conclusion
Physical activity promotion is a core component of high-quality general practice care. Despite recognition of the importance of physical activity for optimal health, the evidence base for effective and sustainable clinical initiatives is still emerging. There are several resources to support GPs in the assessment and prescription of physical activity promotion and exercise care in general practice.
Key points
- Exercise should be considered a fundamental component of high-quality general practice care. Assessing, advocating and monitoring for physical activity as part of ongoing care is recommended.
- Exercise as a ‘vital sign’: exercise and fitness levels can be estimated in practice and this is a feasible component of clinical practice for people with chronic disease.
- Modest improvements in physical activity levels have clinical benefits and should therefore be explored with patients. Approaches such as low-volume HIIT, VILPA and exercise snacks might be more achievable as patients initiate gains in physical activity duration and intensity.
- Resources are available to support GPs to incorporate exercise care into routine consultations. GPs can print or save the links in Table 1 and use platforms such as GoShare to connect patients to the resources. Over 15 exercise-specific clinical practice guides are available through the RACGP Handbook of non-drug interventions, such as exercise for type 2 diabetes, depression and chronic fatigue syndrome.