Male lower urinary tract symptoms (LUTS) secondary to bladder outlet obstruction due to benign prostatic hyperplasia (BPH) represents a significant burden of disease in men globally, afflicting an estimated 30% of men aged >50 years.1 In Australia, LUTS due to BPH affects at least one in every five Australian men aged between 35 and 80 years.2 It is well known that LUTS such as urinary frequency, urgency, urinary incontinence and nocturia are associated with reduced quality of life and depression.3,4
Initial management involves medical therapy; however, up to one-quarter of men discontinue or are non-compliant with their medications due to inadequate relief or side effects.5 In those who fail medical management, there are various surgical options available.
Aim
The aim of this paper is to highlight the various treatment options available today for management of bladder outlet obstruction secondary to BPH and discuss the benefits and potential drawbacks of each.
Lifestyle modification and medical therapy
The European Association of Urology (EAU) guidelines recommend lifestyle and dietary modification as first-line when initially consulting a patient for LUTS.6 Lifestyle advice includes reducing fluid intake during periods when urinary frequency is most inconvenient, such as while asleep or out in public; avoiding diuretic irritants such as caffeine or alcohol and rationalising medications to reduce the urinary side effect profile. Techniques such as relaxation and double voiding techniques are recommended, aimed at relaxing the perineum, improving the posture of the pelvis and taking the time necessary to complete urination.
In men with moderate-to-severe LUTS, alpha 1-adrenoceptor antagonists (α1-blockers) can be offered as first-line medical therapy. Alpha 1-blockers aim to inhibit the effect of endogenously released noradrenaline on smooth muscle cells in the prostate and thereby reduce prostate tone and bladder outlet obstruction.7 Clinical trials have demonstrated an improvement in both storage and voiding LUTS of at least 25% in the majority of patients, and an increase in the maximum flow rate (Qmax) by 20–30%.8,9 The most widely used α1-blockers currently in Australia are tamsulosin and silodosin. The most frequent adverse side effects of α1-blockers are orthostatic hypotension and retrograde ejaculation; however, they are generally well tolerated.
5-Alpha reductase inhibitors (5-ARIs) can provide additional benefit for patients with a significantly enlarged prostate. They are often used in combination with an α1-blocker (eg Duodart). Long-term studies have demonstrated that combination therapy is superior to α1-blocker or 5-ARI monotherapy in improving symptoms and Qmax.10 The 5-ARIs inhibit the action of dihydrotestosterone and induce involution and apoptosis of the prostatic epithelium, leading to prostate size reduction.11 It takes 6–12 months for 5-ARIs to exert their full effect. Studies have demonstrated that 5-ARIs can decrease prostate volume, improve urinary symptoms based on the patient’s International Prostate Symptom Score (IPSS) by approximately 15–30%, and increase Qmax by 1.5–2.0 mL/s after two to four years of treatment.10,12,13 Patients most likely to benefit from 5-ARI have a prostate volume of ≥40 cc or greater (normal range 20–25 cc).14 The potential sexual side effects (reduced libido, erectile and ejaculatory dysfunction) are a deterrent for some patients. An alternative pharmacological option for treating male LUTS is low-dose phosphodiesterase-5 inhibitor (tadalafil). This can be a good option for patients with concurrent erectile dysfunction, or those wanting to avoid side sexual side effects of other medications.
Patients with BPH might present with mixed symptoms, often due to secondary bladder changes that lead to symptoms of detrusor overactivity. Pharmacological options to treat these symptoms include anticholinergics such as oxybutynin and beta-3 agonists such as mirabegron. A detailed discussion of the indication and risks associated with these medications is outside the scope of this article.
Transurethral resection of the prostate
Transurethral resection of the prostate (TURP) removes obstructive prostatic tissue from the transitional zone through the urethra by electrocautery and has been considered as the reference mainstay technique for the surgical management of symptomatic BPH due to its widespread availability and high efficacy. There are two modalities; monopolar or bipolar. Monopolar TURP uses a single active electrode (the loop) at the site of surgery, which transmits energy into the prostatic tissue through the patient’s body to the return electrode pad on the skin surface. This circuit requires a non-conductive hypo-osmolar irrigation medium. In contrast, bipolar TURP is locally confined at the operative site between an active electrode (resection loop) and a return electrode situated on the resectoscope tip. This uses a conductive and physiological irrigation medium such as normal saline, and is favoured by some surgeons as it avoids the risk of transurethral resection (TUR) syndrome, characterised by dilutional hyponatraemia, which can occur in monopolar TURP due to its use of hypo-osmolar irrigation.15,16
In a meta-analysis of 20 randomised controlled trials with a maximum follow-up of five years, monopolar TURP resulted in a significant reduction in IPSS and post void residual volume (–77%) and improvement in Qmax (+162%).17 Both monopolar and bipolar TURP can adversely affect sexual function in men, such as erectile dysfunction and/or retrograde ejaculation, which are linked to worse psychological health outcomes and poorer quality of life.18
Minimally invasive procedures
Various alternatives to TURP have emerged for the surgical management of LUTS secondary to BPH. The major benefits are that many, such as prostatic urethral lift (UroLift), convective water vapor energy (Rezium) and prostatic arterial embolisation (PAE), can be performed with local anaesthesia within the outpatient office setting.19 Although the literature currently suggests that minimally invasive procedures (MIPs) are associated with more modest improvements to LUTS and urinary flow, and higher rates of clinical failure requiring secondary intervention, there is growing popularity in favour of these interventions as they avoid adverse side effects to erectile and ejaculatory function, which can occur with medical therapy and TURP.20,21 Table 1 summaries the mechanism of action, patient selection criteria and potential side effects of each MIP.
| Table 1. Properties of each minimally invasive procedure |
| Technique |
Mechanism of action |
Indications and patient selection criteria |
Side effects |
Availability in Australia |
| Holmium laser enucleation of the prostate (HoLEP) |
Pulsed solid-state laser to resect the transitional zone of the prostate using anatomical planes, then morcellation of this tissue inside the bladder to enable endoscopic extraction |
BPH of any size including prostate size >200 cc, which previously needed open surgery22,33 |
Longer operation times, no significant differences in urethral strictures and stress urinary incontinence rates with TURP34,35 |
Private hospitals and some tertiary public hospitals |
| Photoselective vaporisation of the prostate (PVP) |
Deliver high-energy green light energy to rapidly vaporise the prostatic adenoma |
Suitable for men with prostate size <100 cc. Promising in patients at high risk of bleeding such as those on anticoagulation17 |
Side effect profile on urinary and sexual function comparable to TURP17 |
Private hospitals and some tertiary public hospitals |
| Prostatic urethral lift (UroLift®) |
Involves placement of several retractors into the prostatic lobes to increase the urethral opening, without the use of electrocautery or dissection |
Men with LUTS interested in preserving ejaculatory function, with prostate size <70 cc and no middle lobe
Can be performed in an office setting under local anaesthesia and provide rapid relief of LUTS |
Favourable safety profile; minimal perioperative morbidity; preservation of antegrade ejaculation and erectile function, and minimal long-term complications17,18 |
Private hospitals and few public hospitals |
| Water vapour therapy (Rezum) |
Uses thermal energy in water vapour created by radiofrequency to trigger prostatic necrosis. Injections of water vapour are administered using a treatment needle via cystoscopy |
Indicated for men with a prostate volume of ≥30 cc and enlargement of central zone and/or median lobe |
Favourable safety profile; minimal perioperative morbidity; preservation of antegrade ejaculation and erectile function, and minimal long-term complications36 |
Private hospitals and few public hospitals |
| Aquablation |
Resects prostatic parenchyma using a high velocity waterjet using ultrasound guidance |
Effective in men with prostate size >100 cc28 |
Risk of postoperative bleeding is lower than TURP, but slightly higher than HoLEP; preservation of antegrade ejaculation and erectile function28 |
Not currently available |
| Prostate artery embolisation (PAE) |
Selective embolisation of appropriate prostatic artery to induce tissue necrosis |
Patients with moderate-to-severe LUTS
Those willing to accept less optimal outcomes compared with TURP |
Post-PAE syndrome; urinary retention, transient rectal bleeding, pain, haematuria and UTI
Inadvertent embolisation of the bladder, corpus cavernosum, or anus, leading to ischaemia |
Private and public hospitals with interventional radiology |
| BPH, benign prostatic hyperplasia; LUTS, lower urinary tract symptoms; PAE, prostatic arterial embolisation; TURP, transurethral resection of the prostate; UTI, urinary tract infection. |
Holmium laser enucleation of the prostate (HoLEP) uses a laser to resect the transitional zone of the prostate from the verumontanum to the bladder neck using anatomical planes. This is followed by morcellation or grinding of this tissue inside the bladder to enable endoscopic tissue extraction for histopathological analysis. HoLEP has great versatility in the size of prostate that can be treated. Previously, patients with prostates >100–150 cc would need open simple prostatectomy to treat their massive BPH. HoLEP provides a minimally invasive alternative for glands as large as 200–300 cc.22 HoLEP offers a lower risk of bleeding and shorter hospital stay;19 however, there is a slightly higher risk of urinary incontinence compared with TURP.
Photoselective vaporisation of the prostate (PVP) (or GreenLight laser Prostatectomy) uses a laser fibre to deliver high-energy green light and rapidly vaporise the prostatic adenoma. Efficacy outcomes comparing HoLEP to PVP in randomised trials were comparable.23,24
Prostatic urethral lift (PUL; Urolift®, Teleflex Inc., Pleasanton, CA, USA) involves deploying non-absorbable implants, which act to compress BPH to establish a large calibre urethral channel (Figure 1). Depending on the size and shape of the prostate, a variable number of implants (typically two in each side of the prostate) are used. UroLift® can be performed under local anaesthesia in an office. It is associated with a faster recovery time and preservation of sexual function.
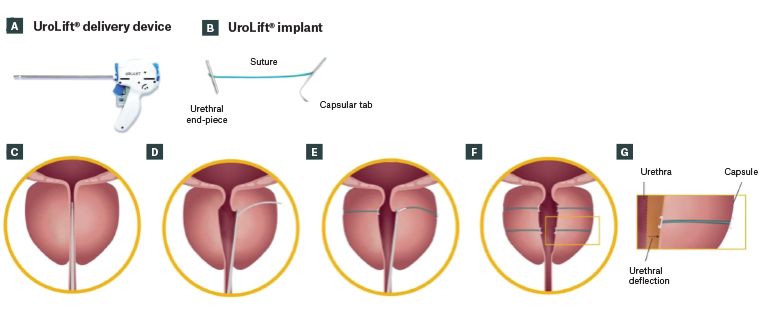
Figure 1. The UroLift System is comprised of two main components: (A) the UroLift delivery device and (B) the UroLift implant. The delivery device is designed to access the prostatic urethra and deliver one implant through the lobes of the prostate. The implant consists of a capsular tab (CT), made from nitinol (nickel titanium alloy), connected by a monofilament polyethylene terephthalate suture to the urethral end-piece (UE), made from stainless steel. The materials used in the implant are made of chemically and biologically inactive materials, commonly used in other implants. Details of the prostatic urethral lift procedure are as follows: (C) under cystoscopic guidance, the delivery device is introduced through the sheath and is used to compress the prostate lobe. (D) A 19-gauge needle that houses the implant is deployed through the prostatic lobe and capsule. Upon retraction of the needle, the CT is deposited with a suture under tension. (E) The implant is secured by deployment of the UE and excess suture is cut. (F) Additional implants are delivered as required. (G) The glandular stromal tissue of the prostate is compliant and more easily compressed outwardly resulting in the opening of the prostatic urethra.
Reproduced from Roehrborn CG, Chin PT, Woo HH. The UroLift implant: Mechanism behind rapid and durable relief from prostatic obstruction. Prostate Cancer Prostatic Dis 2022;25(1), with permission from the Nature Publishing Group.37
Water vapour thermal therapy (Rezum System, Boston Scientific, MXG, Massachusetts) uses radiofrequency to generate convective water vapour energy, which is delivered to obstructive adenomatous tissue to induce prostatic necrosis (Figure 2). Injections of vapour are delivered transurethrally.25 It can be performed under local anaesthetic in the outpatient setting. The Rezum System is popular for its preservation of sexual function.26 Its drawback is that patients need to have a urethral catheter after surgery, often for up to a week.
 Figure 2. Rezum system delivery device and needle.
Figure 2. Rezum system delivery device and needle.
Reproduced from Woo HH, Gonzalez RR. Perspective on the Rezūm® System: A minimally invasive treatment strategy for benign prostatic hyperplasia using convective radiofrequency water vapor thermal therapy. Med Devices (Auckl) 2017;10, with permission from Dovepress.38
Aquablation uses the principle of hydro-dissection to resect prostatic parenchyma using a high velocity waterjet under real-time transrectal ultrasound guidance, without the need to generate thermal energy. Haemostasis is achieved with a Foley balloon catheter on light traction, diathermy or low-powered laser. It is an effective treatment for prostates >100 cc.27,28
Prostatic arterial embolisation (PAE) can be performed as a day procedure with local anaesthesia and involves femoral or radial artery puncture guided by digital subtraction angiography.29 The appropriate prostatic artery is selectively embolised to induce tissue necrosis. PAE has longer procedural time and is less effective than TURP at improving symptoms and urodynamic parameters such as flow rate.30 However, PAE might be associated with fewer adverse events and shorter length of postoperative hospital stay compared with TURP.31 It is particularly well suited to patients who would not otherwise be fit for surgery.
The decision to undergo TURP or a MIP can be guided by the balance of benefits and harms based on patients’ values and preferences. Although men prefer a quick relief with stable, long-term results, many are mindful of the risks of opting for surgical intervention such as disturbance to sexual and urinary function.32 Although the literature is in favour of MIPs in terms of fewer adverse side effects to sexual and urinary function, many studies to date have limitations in their internal validity and generalisability. GPs can optimise care to patients suffering from symptomatic BPH through shared decision making, taking into consideration their preferences and values32 and prescribing medical therapy or referring to a urologist for surgical intervention where appropriate.
Conclusion
There are various options available today for managing LUTS secondary to bladder outlet obstruction due to BPH, ranging from lifestyle modification, medical therapies and surgical interventions, including TURP and MIPs. Although not as effective in the long term in dramatically improving a patient’s LUTS compared with TURP, MIPs are proving to be popular due to their low side effect profile and ability to be performed as a day case procedure in an office setting. GPs should follow a stepwise pattern of management, commencing with lifestyle modification advice and consider a medical agent that is appropriate for the age, preferences and sexual habits of the patient. A referral to a urologist is recommended for persisting bothersome symptoms despite medical therapy, for consideration of surgical intervention. An awareness of the various MIPs available today can be helpful when counselling patients on treatment options for LUTS due to bladder outlet obstruction.
Key points
- LUTS, due to BPH, globally affects 30% of men aged >50 years, and in Australia, affects one-in-five men aged between 35 and 80 years, leading to reduced quality of life and depression.
- Lifestyle modifications and a1-blockers are initially recommended, with 5-ARIs offering additional benefit for patients with a significantly enlarged prostate (with potential sexual side effects).
- Referral to a urologist is recommended for consideration of surgical intervention in men with persisting bothersome symptoms despite medical therapy, or who do not adhere with medical therapy.
- TURP remains the standard of surgical intervention, demonstrating significant improvement in urinary symptoms, but with potential adverse effects on sexual function.
- Emerging minimally invasive options including UroLift®, Rezum and PAE offer alternatives to TURP, and are proving to be popular due to their low side effect profile, shorter inpatient stay and ability to be performed on co-morbid populations.