Foreign bodies (FBs) in the ears and nose are prevalent clinical presentations commonly seen among paediatric patients and managed by general practitioners (GPs), emergency physicians and otorhinolaryngologists. Patients might present with relatively minor symptoms, but the complications of some FBs can lead to serious outcomes, such as infections and deformities. Therefore, the primary goal is safe, timely and complete FB removal, necessitating clinicians to select appropriate methods of retrieval and to identify cases requiring specialist referral.
Although the most suitable method depends on FB characteristics, patient compliance, available medical equipment and the proficiency of the clinician, clinical guidelines for specialist review are lacking, posing challenges in patient selection for referral. This article offers a standardised approach to managing aural and nasal FBs, drawing on local experience and clinical data from a tertiary paediatric centre, while highlighting key clinical parameters that warrant specialist review.
Aims
The aims of this article are to provide a standardised approach to FB removal in the paediatric population for GPs and emergency physicians; outline the pros and cons of common retrieval methods, and factors that increase the risk of complications; and to suggest indications for referral to emergency departments (EDs) and otorhinolaryngology.
Recommendations
Local data
A clinical audit was conducted at a Queensland paediatric tertiary centre from August 2022 to February 2023 for patients referred to otorhinolaryngology with aural and nasal FBs. In all, 144 cases were identified, aged between one and 16 years with a mean age of 5.2 years (Table 1). The most common FBs were beads and various forms of plastic, and none involved button batteries or magnets. Referrals to otorhinolaryngology were mostly from EDs (Figure 1). Among all patients, 37–53% required FB removal under general anaesthesia, highlighting a subset of difficult cases unsuitable for management in the community that had been appropriately referred to otorhinolaryngology. The remainder of cases were adequately managed in the outpatient setting with the use of equipment as shown in Figure 2.
| Table 1. Summary of local data in South East Queensland, August 2022 – February 2023 |
| |
Aural FB |
Nasal FB |
| No. patients |
|
|
| Mean (±SD) age (years) |
|
|
| Most common FB |
- Plastics (16%)
- Beads (11%)
- Plant (7%), crayon (7%), playdough (8%)
|
- Foodstuff (27%)
- Plastics (22%)
- Bead (12%)
- Foam (8.5%), playdough (8%)
|
| Laterality |
- Right, 42
- Left, 31
- Both, 12
|
|
| Source of referral |
- GP, 11%
- GP and EDA, 16%
- ED, 71%
- Private, 2%
|
- GP, 7%
- GP and EDA, 10%
- ED, 83%
|
APatients referred to the emergency department (ED) by their general practitioner (GP) and then referred to the ear, nose and throat department.
FB, foreign body; SD, standard deviation. |

Figure 1. Source of referral to otorhinolaryngology.
ED, emergency department; FB, foreign body; GP, general practitioner.
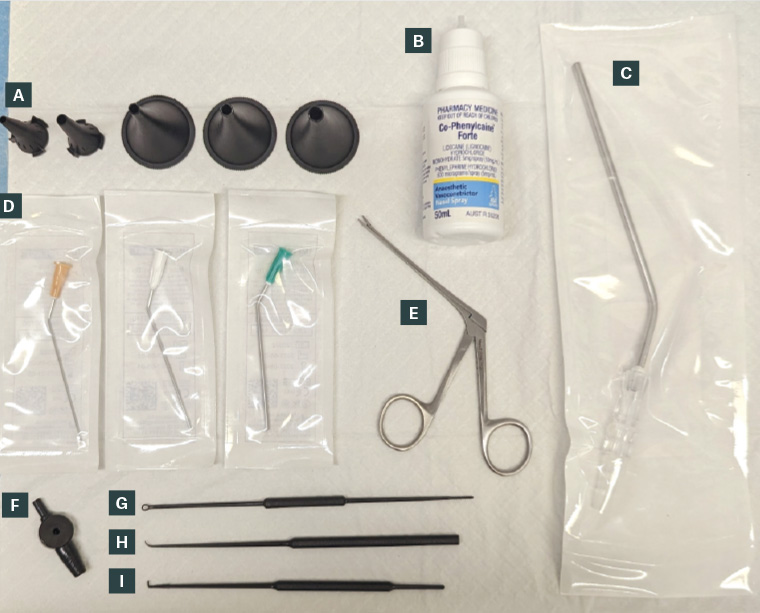
Figure 2. Commonly used tools for retrieval. (A) Aural speculums. (B) Co-Phenylcaine (phenylephrine and lidocaine) spray (ENT Technologies). (C) Frazier sucker. (D) Microsuction tubes. (E) Alligator forceps. (F) Suction controller. (G) Wax curette. (H) Rosen/curved hook. (I) Right-angled hook.
Approach to FB removal
Preparation
Initial consultation should cover FB type, time and method of insertion and associated symptoms, such as pain, bleeding and discharge. Relevant comorbidities, such as diabetes, coagulopathy or neuropsychiatric conditions that might impact compliance, should also be noted. Informed consent, either verbal or written, from the patient and their parents should include the necessity of removal, immobilisation, expected discomfort and potential complications. The examination should be brief to confirm the type and location of the FB and to determine the most appropriate retrieval approach.1–3 From local experience, patients tend to benefit from having the procedure explained to them throughout and receiving constant reassurance to maintain compliance.
The success rate is highest on the first attempt, so adequate visualisation and having the necessary equipment available are imperative (Figure 2).1–5 A headlight is an inexpensive source of illumination that frees up both hands for instrumentation. The ear should be pulled superoposteriorly and the largest speculum that fits comfortably in the canal should be used to maximise illumination. A nasal thudicum (if available) or elevating the nasal tip with the patient’s head extended will help visualise the anterior portion of the nasal passages. The patient should be supine on the bed or on the parent’s lap, with the assistant stabilising the head. Patients aged under two years can be immobilised by swaddling in a sheet, but older children who are non-compliant will likely require sedation.4,5 Distractions like videos or familiarising the patient with the equipment can be beneficial, although instruments with sharp ends should be avoided because these tend to evoke anxiety.
Topical agents such as co-phenylephrine and lignocaine (Co-Phenylcaine Forte, ENT Technologies) are useful in the case of nasal FBs when applied at least five minutes prior to the retrieval attempt for sufficient topical anaesthesia and local vasoconstriction, minimising pain, bleeding and nasal secretions as a result.1,4 The dosage must be age adjusted, and the spray is not approved for use in those aged under two years. Moreover, co-phenylcaine is not advised in aural FBs due to risks of injury to the canal and the tympanic membrane.
Aural FBs
The external auditory canal (EAC) extends from the pinna to the tympanic membrane (TM) and fully develops to approximately 2.5 cm by the age of nine years.6,7 The EAC comprises a cartilaginous outer third and a bony inner two-thirds. FBs are commonly found at two natural narrowings: the bony–cartilaginous junction and immediately lateral to the TM.7,8 Rarely, they might also be found at the anteroinferior tympanic sulcus, often obscured by the anterior canal wall. Adult EACs have various sigmoidal shapes, whereas paediatric canals are straighter.7
The gold standard should be a combination of microsuction and alligator forceps (Figure 2D–F). Although microsuction devices are rare in the community, alligator forceps are more readily available and can remove most graspable FBs. Alternatively, a wax curette or right-angled and curved hooks (Rosen needle) are more commonly available, and the latter two can be fashioned from the end of a hypodermic needle.9 A wax curette is best suited for viscous FBs (eg clay), whereas the hooks can go through or around the FBs and brought forward; however, this requires the patient to be cooperative and stationery to avoid iatrogenic injuries.
Irrigation with warm water has limited application. Its use is contraindicated for batteries due to associated alkali injury, in hygroscopic FBs (eg vegetable matters), in grommets and when the integrity of the TM cannot be verified, which is often the case.1,4,9 Furthermore, irrigation might also push the FB deeper along the canal and predispose the patient to otitis externa.
Live insects in the EAC should first be killed by pouring inert oil (eg olive oil, baby oil) into the canal, then removed later.1,4,9 Superglue (cyanoacrylate) and hydrogen peroxide solutions have been mentioned in the literature, but they are generally not recommended due to the high risk of iatrogenic injuries.1,9 A summary of recommendations is provided in Table 2.
| Table 2. Common methods of aural foreign body removal |
| Method |
Suitable for … |
Avoid in … |
RecommendationsA |
| Microsuction |
- Organic or friable materials (eg food items, insects)
- Round objects (if adequate seal can be achieved)
- Small, non-occlusive and light objects
|
- Near the TM (if performed with headlight)
- TM perforation
|
Strong |
| Alligator forceps |
- Hard materials (eg plastics, insects)
- Objects with graspable edges or those that can be grasped whole
|
- Friable or viscous materials (eg clay, mushy food items)
- Round objects
|
Strong |
| Right-angled and curved hooks |
- Objects with a hollow centre (eg beads)
- Round objects without graspable edges
|
- Friable or viscous materials
|
Moderate |
| Wax curette (Jobson–Horne) |
- Friable or viscous materials (eg clay, wax)
- Round or smooth objects
|
- Objects with sharp points or edges
- Objects near the TM
|
Moderate |
| Irrigation |
- Small, loose objects or particles
|
- Batteries
- Hygroscopic materials (eg vegetable, polystyrene balls)
- TM perforation or grommet in situ
|
Low |
ARecommendations are based on literature and local experience.3–5
TM, tympanic membrane. |
Nasal FBs
The nose comprises a pair of cavities extending from the nares to the postnasal space, divided by the vertical nasal septum and subdivided by three sets of horizontal nasal turbinates. FBs are commonly found between the septum and the inferior or middle turbinates, or between the nasal floor and the inferior turbinates.2,10,11
FBs in the anterior nasal cavity might simply require nose blowing. If the patient is unable to perform this, a positive-pressure technique (‘mother’s kiss’) can be used, especially in the first 12 hours after insertion. This requires the patient seated with the contralateral nostril occluded, and the parent rapidly blowing into the patient’s mouth to force the FB out.1,5,11
Nasal FBs tend to be between two structures, so a wax curette or right-angled or curved hooks are often positioned behind the FB and pulled forward. Head stabilisation is thus imperative to minimise mucosal and iatrogenic injuries, because the area is well vascularised and minor bleeds are common. Both nasal passages must be re-examined after the initial retrieval to ensure all FBs are removed.
Irrigation is not recommended due to the risk of aspiration, particularly in a distressed patient.4,11,12 The theoretical risk of aspirating a nasal FB is not warranted in a healthy child with intact airway reflexes and has not been reported in the literature to date.12,13
In patients where an FB is suspected but not visualised, the parents should be counselled on key symptoms, such as unilateral mucopurulent discharge, malodour and unilateral epistaxis, and to return if concerned. A summary of recommendations is provided in Table 3.
| Table 3. Common methods of nasal foreign body removal |
| Method |
RecommendationsA |
| Microsuction |
Strongly recommended for most objects in the anterior nasal cavities, as well as for clearing nasal secretions |
| Alligator forceps, curved hooks, curettes |
Moderately recommended contingent on the shape and location of the object, patient compliance and clinician expertise |
| Irrigation |
Not recommended |
| Positive-pressure technique |
Obstructive objects in compliant patients |
| ARecommendations are based on literature and local experience.3–5 |
Complications
Common complications include local trauma, infection, bleeding and TM perforation. Multiple failed attempts, non-graspable FBs and prolonged duration of FB impaction increase the risk of complications.5,7,12–15 Minor trauma and bleed tend to settle spontaneously and do not necessitate antibiotic use. For aural cases with suspected or confirmed infection, topical antibiotic drops are recommended, whereas nasal cases should receive saline nasal spray or flush, with consideration of intranasal steroid spray and oral antibiotics. Patients with TM perforation should only receive ciprofloxacin-containing ear drops because other formulations might cause ototoxicity.
When to refer
All patients with suspected or confirmed button batteries and disc magnets must be referred to otorhinolaryngology immediately because these not only cause immediate injuries, but also lead to further injuries hours after removal.1,4,5,16,17 Park and Burns’ article includes a flow chart specific to button battery ingestion that highlights the importance of early recognition and removal.17 Patients with sharp, non-graspable or penetrating FBs intolerant to examination might require presentation to the ED to facilitate removal under sedation and consultation from otorhinolaryngology.1,4,5,9,16 For non-urgent cases, including inert FBs, asymptomatic cases and a lack of equipment or clinician experience, the tertiary paediatric hospital in Queensland has an email address designated to receive referrals for FBs and nasal fractures, separate from the central referral system (kidsent@health.qld.gov.au). It is monitored by the otorhinolaryngology nurse and has been effective in providing timely treatment to patients with FB. Protocols will likely differ in other states, so it might be prudent to see whether similar streamlined referral pathways exist locally. The patient should be informed of the referral that might necessitate long-distance travel. A flow chart of when to refer to ED and otorhinolaryngology is provided in Figure 3.
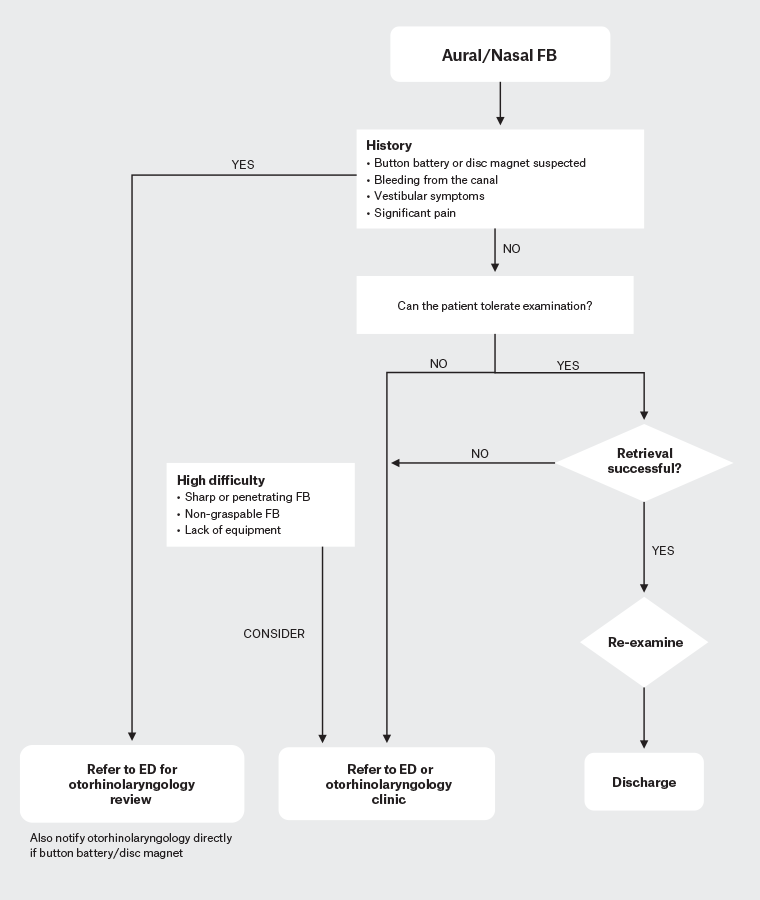
Figure 3. Flow chart of decision making for foreign body (FB) removal and when to refer. Click here to enlarge
ED, emergency department.
Conclusion
FBs in the ears and nose are common clinical presentations in paediatric cases faced by GPs, emergency physicians, and otorhinolaryngologists and require timely and safe removal to prevent complications. The success rate is highest on the first attempt, so preparation and the ability to use different techniques are strongly advised. Urgent referral to otorhinolaryngology is necessary for button batteries, significant infections, failed attempts, lack of expertise or equipment and cases requiring sedation.
Key points
- FBs in the ears and nose are common paediatric presentations seen in general practice and EDs.
- A standardised approach to FB removal involves appropriate history taking, patient positioning and equipment preparation.
- A combination of microsuction and alligator forceps is recommended as the gold standard for aural and nasal FBs.
- The risk of complication is primarily increased by multiple failed attempts at FB removal.
- Urgent referral to otorhinolaryngology is necessary for button batteries and disc magnets.