Modern Australian healthcare systems face mounting economic and logistical changes, with the recent Intergenerational Report estimating that health spending is projected to grow from 4.2% of gross domestic product (GDP) in 2022–23 to 6.2% of GDP in 2062–63.1 A significant contributor to this healthcare cost is increasing numbers and complexity of outpatient consultation for chronic disease. The concept of shared care has emerged as a solution for clinicians, administrators and policymakers.2,3 Shared care is a healthcare model that recognises the limitations of a single healthcare provider and aims to improve the quality and comprehensiveness of care through joint participation of primary and specialty physicians in planned delivery of care through enhanced information exchange.2,4 This includes shared care plans, direct messaging (particularly to cancer nurses), educational support, clinical decision aids and more.4 Although traditional paper-based shared care models intend to combine the expertise of general practitioner (GP) and hospital specialists, in reality, they face challenges, especially in rural areas, prompting the need for more efficient care models and patient-centric approaches that transcend these barriers.
The future role of shared care in the Australian healthcare system cannot be overstated. With an ageing population, demographic shifts and the increasing prevalence of multiorgan chronic diseases, the demand for healthcare services is growing.1 As the healthcare system faces this mounting pressure, more efficient and cost-effective models of care will become increasingly important.1 Shared care alleviates burden on the healthcare system by bridging existing systems and also provides patient-facing interfaces that allow the flexibility and accessibility patients expect in modern healthcare.
The convergence of shared care and digital technology is a promising avenue that has the potential to revolutionise healthcare practices.4 With the rapid advancement of digital technologies (near complete primary care penetrance),5,6 including electronic health records (EHRs), telemedicine, health apps and artificial intelligence (AI), we are poised to explore the latest innovations and updates in digital shared care approaches.
Aim
This article aims to explore the contemporary Australian eHealth shared care landscape.
The digital transformation of healthcare
Healthcare has undergone a significant digital transformation in the last decade. This has occurred through the proliferation of eHealth, which can be defined as the delivery and support of health via the secure use of information communication technologies (ICT).4,7,8 This encompasses a wide range of technologies, from mobile applications (mHealth) and telemedicine to EHRs and internet-based services.4,9,10 This transformation has laid the groundwork for advanced shared care models that leverage technology to enhance patient care coordination.4
In 2021, more than 350,000 mHealth applications were readily accessible for free download and usage (www.statista.com/statistics/889582/mhealth-apps-market-size-forecast-by-type-in-the-us).9,10 In a 2018 survey of Australian GPs, it was found that 44% recommended mHealth applications to patients on at least a monthly basis.6 However, despite this widespread use, a significant lack of high-quality evidence was noted for the majority of available health apps.10 Outcome measures in published eHealth literature tend to favour ‘soft’ or process-oriented outcomes over clinical endpoints, highlighting a gap between the rapid adoption of technology and the evidence supporting its benefits.10 Concerns remain over the implementation of technologies before sufficient evidence of their benefits and harms is available.10 An overview of systematic reviews on mHealth applications conducted in 2018 found that only 23 of them had data supported by randomised controlled trials (RCTs), and among these, only 11 out of 23 reported any significant and clinically meaningful outcomes linked to their usage.10
The Australian eHealth landscape
Australia has made significant strides in eHealth adoption, with almost universal clinical computerisation in general practice.6 The most recent Royal Australian College of General Practitioners’ (RACGP) survey on digital adoption (2018) showed that 87% of GPs in Australia are entirely digital with no paper records.6 This highlights that Australia’s primary care is among the leading countries globally when it comes to eHealth integration. More granular results include that 98% of GPs regularly employ desktop computers, 89% access the internet daily and two-thirds of GPs recommend mHealth applications to their patients.6 However, despite widespread internet access and a recommendation by the RACGP that electronic communication should be the default method, less than half of all GPs use secure message delivery, and older communication methods, like fax, phone and mail, were shown to predominate.6 The reasons for the delay in adoption of newer communicative technologies by both the senders and recipients are varied,6,11 but predominating features among healthcare providers include the cost of technology, the learning curve for adoption of technological features, data safety assurances, concurrent receiving technologies in tertiary care and ease of access via incorporation into the practice electronic medical record software.6,12 However, certain versions of general practice software, such as Best Practice, now integrate secure email services for referrals and communication with specialists, along with secure messaging for patients to receive results and reminders (eg author, JC’s practice). This has rendered fax and mail slower, less secure and more expensive options. However, challenges remain for patients without email or mobile messaging capabilities, particularly elderly patients, and there are ongoing concerns about spam risks associated with electronic message links.
eHealth in the rural setting
Digital communication technology has also been shown to enhance healthcare accessibility in rural communities.13,14 Australia’s rural and remote population is widely distributed, with many using eHealth for primary care as well as specialist care.15 LeBlanc et al interrogated eHealth’s success in Australia and Canada, through a scoping review, and found reduced anxiety, disruption on family life, improved follow-up rates and improved recovery time.14
One key improvement with widespread digital uptake has been universal access to patient education resources, which have been shown to improve patients’ chronic disease understanding, participation and management plan compliance.16 However, despite this ease of access, patients can experience information overload, with difficulty differentiating the quality of online resources.17 Although government organisations have well-written, evidence-based information that is readily accessible for patients, those with reduced health literacy can often become confused or anxious with the complexity of the information. This highlights the importance of repeat visits and consistent channels for communication.16
eHealth technologies for management of chronic disease
Barriers to the evidence-based chronic care model of health have been well described (Figure 1).18 eHealth is well placed to directly address such barriers, with resultant improved chronic disease management (Table 1). These interventions include continuous education combined with audit and feedback, collaborative team-based interventions, and advanced information technology-based systems, including clinical decision support (Figure 1).4,18 These technologies seek to address key barriers to healthcare access, including practical accessibility challenges, negative prior experiences with healthcare services, stigmatisation and adverse interactions with staff and fellow patients. A key technology to facilitate this is remote patient monitoring (RPM), which has shown utility across a range of chronic diseases.19 However, despite well-established, evidence-based local guidelines supporting integrated eHealth chronic disease management, Australian implementation has been limited.6 The essential aspects to functional EHRs, particularly in shared care, include shared EHRs, electronic consultation and referrals, electronic patient portals with messaging systems and telehealth systems for virtual consultation.4,12
| Table 1. Barriers to implementation of the chronic care model and potential eHealth solutions |
| Barrier to the chronic care model |
Potential eHealth solution |
- Complexity in communication resulting in large amount of phone, fax and telephone communications (particularly in obtaining approval for care plans and reporting results/interventions)
|
- Online shared disease record
- Secure electronic messaging
|
- Complexity in constructing meaningful, evidence-based and up-to-date care plans
|
- Clinical decision support systems offering automated, up-to-date, personalised care plans
|
- Complexity in keeping track of what each person in the care team is doing over time
|
- Online shared disease record and task management system
|
- Burden of regular review and follow-up, including logistical issues in recalling patients
|
- Electronic alerts and secure electronic messaging
- Automated treatment plans and scheduling
|
- Limited means of providing support for patient self-management
|
- Electronic patient portals with secure messaging to treatment providers
|
- Administrative burden in meeting Medicare documentation requirements
|
- Clinical decision support systems incorporating automated construction of treatment plans
|
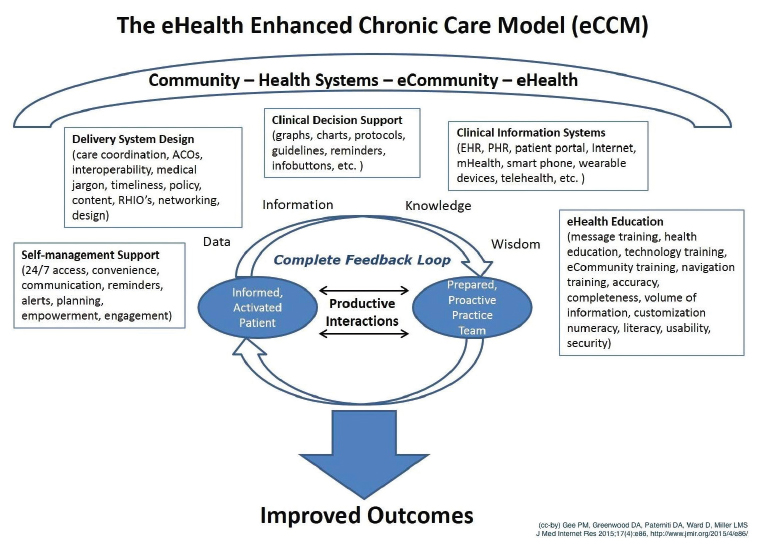
Figure 1. The eHealth Enhanced Chronic Care Model (eCCM). Click here to enlarge
ACOs, accountable care organisations; EHR, electronic health records; PHR, personal health records; RHIO, regional health information organisations.
Reproduced from Gee PM, Greenwood DA, Paterniti DA, Ward D, Miller LM. The eHealth enhanced chronic care model: A theory derivation approach. J Med Internet Res 2015;17(4), with permission from JMIR Publications Inc.
Shared electronic health records
A shared EHR refers to a cloud-based record that all members of a healthcare team can access, with the primary goal of delivering integrated multidisciplinary care. Shared EHRs aim to improve collaboration between primary and specialist care providers. Studies involving shared EHRs have shown improvements in clinical outcomes, such as better glycaemic control and weight reduction in diabetes management.20
As of January 2019, 90.1% of Australians had an EHR created automatically (through My Health Record), with the remainder choosing to opt out. Although Australia has made progress in this area with the My Health Record system (currently 23.7 million records or 98% of Australians), there are ongoing issues with specialist uptake (only 300,000 instances of specialist use since inception), technical usability and document restrictions.21,22
Shared records: Key building blocks
Several key building blocks contribute to the success of shared records, ensuring semantic interoperability, standardisation of terminology, adherence to industry standards such as fast healthcare interoperability resources (FHIR) and robust governance structures. Semantic interoperability refers to the ability of different systems and organisations to exchange data and interpret the meaning of that data accurately.23 Achieving semantic interoperability involves using common data models, standards and standard terminology to ensure that information is understood and captured consistently, and exchanged in a uniform and meaningful way between stakeholders.23 FHIR is such a set of standards for exchanging healthcare information electronically.24 FHIR defines a modular approach to data exchange, using resources such as Patient, Practitioner, Observation and Condition, which can be easily accessed and shared across different healthcare information technology (IT) systems.24 Establishing robust data stewardship and governance is critical for maintaining the integrity, security and quality of shared records.25 This includes defining data ownership, access controls, data quality standards and privacy protections to ensure that patient information is handled responsibly and ethically.25 Critical to retrofitting a heterogenous digital landscape like Australia is a reliable infrastructure for data exchange, including application programming interfaces (APIs), data integration platforms and interoperability frameworks.26 The recent national healthcare interoperability plan has placed integrating healthcare systems as a critical step in the digital health infrastructure pipeline.26
Secure electronic communication, consultation and referral
The RACGP recommends electronic communication as a standard in primary care.11,27–29 Experience across multiple shared care platforms has found communication tools to be the most valuable aspect of shared care for both clinicians and patients.30–37 Of these, patient-direct messaging with specialised nursing staff within business hours has been shown to reduce patient anxiety and treatment uncertainty.30–35 Building platforms to further improve inter-clinician communication will be an essential part of future digital shared care platforms.
Electronic referral and consultation systems have shown promise in reducing waiting times and improving care access compared to standard systems.38,39 However, concerns persist about usability and the potential for confusion surrounding tasks and responsibilities.38 Electronic specialist consultation allows GPs to seek online opinions from specialist colleagues. Although the published evidence on this practice is limited, it has seen successful implementation in remote northern Canada.40 Notably, these services have achieved high user satisfaction, reduced wait times for specialist review and significant cost savings, estimated at $1000 per consultation.40 Although patients and primary care providers believe eConsults could enhance the quality of care, 43% of specialists have expressed concerns that eConsults might compromise the quality of care.41,42 A recent eight-year Brazilian study demonstrated eConsults as an effective initial assessment tool, with 223,734 specialist virtual reviews providing satisfactory or very satisfactory input in 90% of cases.43
Electronic patient portals
Electronic patient portals offer patients access to their medical records and electronic communication with healthcare providers, improving patient satisfaction and convenience.27 However, their effectiveness in improving clinical outcomes varies across different patient demographics and clinical scenarios, and their benefits might be most significant in cases where there is an existing physical relationship between patients and clinicians.28 In a younger age group (16–24 years), the combination of email communication and in-person consultations not only increased autonomy and empowerment but also fostered improved trust with familiar healthcare providers.44 The most extensive ‘patient portal’ implementation to date is the ongoing Australian My Health Record system, with 98% of Australians enrolled (23.7 million records). However, of this, only 24% (5.74 million records) have been reviewed by patients.22 This is likely due to arduous registration processes, but further work must be done to clarify the reason for its underutilisation as well as its clinical effectiveness.45
Telehealth
Telehealth was first described in 1879 when an article in The Lancet proposed the idea of using telephones to reduce unnecessary patient appointments with the goal of reducing geographical barriers and improving patient access to care.46,47 Telehealth (initially phone and now video call) has gained widespread acceptance and satisfaction from both patients and healthcare providers,48 and has the potential to save patient travel time and costs, decrease time missed from employment, and reduce environmental pollutants, particularly in rural and remote areas.49 On systematic review, video calls appear to be superior when visual information is required or patient engagement is linked to clinical outcomes.50 In rural settings, telehealth has widely been accepted as a clinical adjunct to follow-up care and delivery of results, reducing the burden of long road travel, allowing prompt delivery of information and reducing formal face-to-face reviews to situations where the clinical need arises.51 Although studying its clinical effectiveness is limited by variations in healthcare specialities, systems, technology, populations and implementation strategies,49,51–53 rapid technological shifts post-COVID suggest that in the right context, it does not compromise effectiveness of clinical care.53
Future direction and innovations in digital shared care
A robust digital shared care platform could better enable future technologies to address growing challenges in Australian care delivery. Properly directed AI and machine learning are being integrated into shared care decision-making tools, diagnostics and treatment planning.54 Logic-driven platforms with data-driven insights to support healthcare providers will be important for rapid generation of personalised treatment plans. Continuous monitoring through wearable devices and Internet of Things (IoT) sensors will likely communicate with these platforms, offering real-time data sharing among healthcare teams.55 Patients can currently use devices such as smartwatches to track vital signs, activity levels and medication adherence.55 Integrating this real-time data into shared care platforms could transform both early detection and allow personalised, streamlined care.
Implementing digital shared care
Successful digital shared care will need to integrate with existing healthcare systems, adhere to data privacy regulations, provide easy access to health information, and involve patients in decision-making. Encouraging health data sharing will empower patients and make them active participants in their healthcare journey (Figure 2).12 Upskilling of some doctors and patients might be required for them to have confidence in using digital health platforms. Importantly, such platforms will need funding models that remunerate clinicians for digital care and platform engagement. One possible solution is capturing data from tasks completed in the hospital setting through the shared care platform and autogenerating multidisciplinary care plans that align to Medicare Benefits Schedule (MBS) requirements for primary care billing. Such remuneration plans are required for effective multidisciplinary collaborations needed for successful implementation of integrated patient-centred shared care.
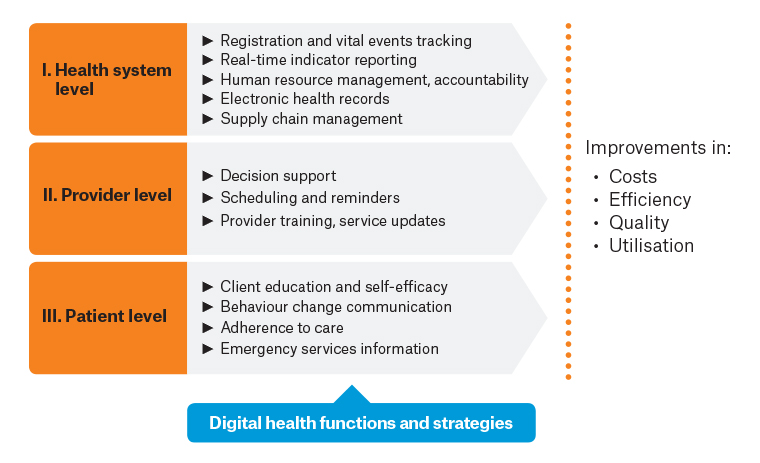
Figure 2. Priority areas for eHealth development and potential benefits.
Reproduced from the World Health Organization (WHO). Monitoring and evaluating digital health interventions, with permission from the WHO, 2016.
Conclusion
As we journey further into the 21st century, digital shared care will play an increasing part in the healthcare system, improving the level of healthcare personalisation and accessibility. The convergence of digital technology and shared care promises more efficient, patient-centric healthcare systems. Australia’s unique healthcare challenges, including geographical vastness, rural populations and a burden of chronic diseases, make it an ideal testing ground for innovative care models. Although challenges like data privacy and interoperability persist, they are not insurmountable. By following best practices, prioritising patient-centred care and involving policymakers, Australia is well positioned to lead the way in the digital transformation of shared care.
Key points
- The Australian healthcare system faces economic and logistical challenges due to an ageing population and an increasing number of chronic diseases, leading to a projected growth in health spending.
- Shared care, which emphasises collaboration between primary and tertiary providers, has emerged as a solution.
- The digital transformation of healthcare in Australia will be increasingly crucial for improving patient care coordination.
- Technologies such as shared EHRs, secure electronic communication, electronic patient portals and telehealth play a significant role in enhancing healthcare accessibility and managing chronic diseases.
- Future inter-electronic medical record integrations hold promise for more efficient and patient-centric healthcare systems in Australia.