Case
A fair-skinned woman, aged 83 years, presented with three rapidly growing, tender lesions (Figure 1). A melanoma-in-situ was removed from her left calf at age 33 years. For the last three decades, she has had one or two keratinocyte malignancies treated per year. Over the last 12 months, the frequency of lesion development has accelerated greatly.

Figure 1. Lesions of the patient case at presentation. (A) Left thumb. (B) Right foot. (C) Left side of the nose.
Question 1
What are the clinical features and probable diagnoses?
Answer 1
The thumb and foot lesions were domed erythematous papules with central keratin plug typical of keratoacanthoma (KA). Squamous cell carcinoma (SCC) was the main differential. The nasal lesion was an erythematous scaling papule. Dermoscopic examination revealed scaling with no observable vessels. Solar keratosis (SK) or intraepidermal carcinoma (IEC) were likely diagnoses, though early SCC was a consideration.
Case continued
All three lesions were managed with shave to deep dermis followed by immediate curettage and cautery. It was anticipated this approach would serve both diagnostic purposes and provide definitive treatment if the provisional diagnoses of KA and IEC were confirmed. The nasal lesion was reported as an IEC arising in a SK. Both the other lesions were KAs. The patient was reviewed three weeks later (Figure 2).
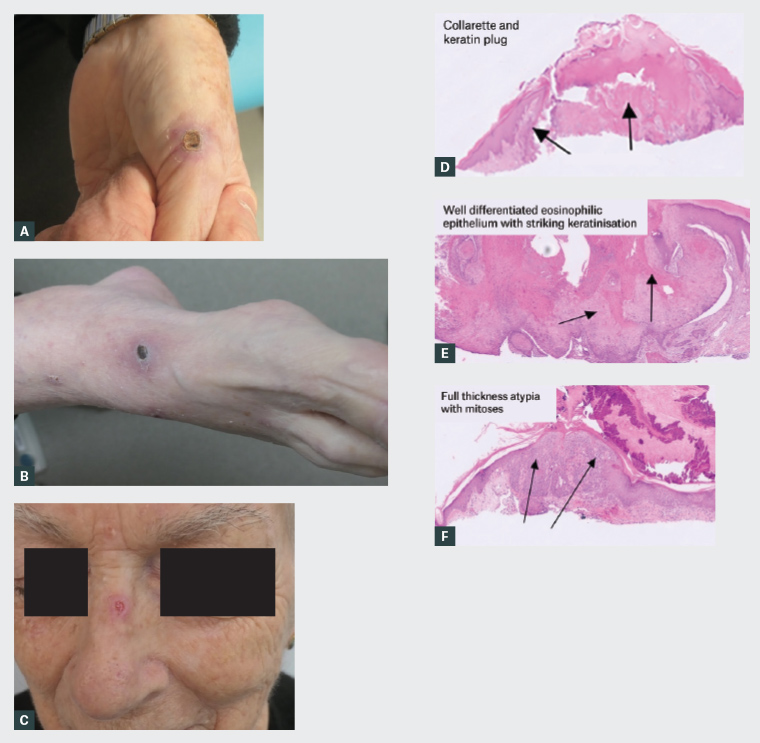
Figure 2. Lesions at follow-up at 3 weeks after initial presentation. (A–C) Healing sites 3 weeks’ post shave, curettage and cautery. (D, E) Histopathology demonstrating keratoacanthoma. (F) Histopathology demonstrating intraepidermal carcinoma.
Question 2
Why was shave and curettage chosen over excisional surgery for these lesions?
Question 3
What factors contribute to a sudden increase in skin malignancy?
Answer 2
Surgical excision is commonly used in managing cutaneous SCC,1 but can impair function, especially over critical sites like joints. Excisional surgery would necessitate immobilisation for optimal healing.2 Given the patient’s age and potential complications, simpler treatment is a reasonable initial approach due to wound healing concerns and complex repair risks.3 This patient had been subjected to multiple hospital admissions and deferment of treatment to another day might have resulted in significant delay.
Shave and curettage, a straightforward same-day procedure with a high cure rate for KA and IEC, was performed. It provides histopathological confirmation, preserves normal tissue, and has simple aftercare with good functional and cosmetic outcomes in photodamaged skin.4 The patient had many lesions treated with this procedure over the years. Histopathology revealing a more aggressive lesion would have been managed by re-excision.
Answer 3
The factors that contribute to a sudden increase in skin malignancy are described in Table 1.
| Table 1. Acquired risk factors of increased non-melanoma skin cancers |
Immunosuppression1
- Bone marrow/stem cell transplant
- Organ transplant
- Leukaemia
- Lymphoma
- Myeloproliferative disorders5
|
Medications6
- Photosensitising medications
- Non-steroidal anti-inflammatory
- Antibiotics
- Tetracyclines
- Fluoroquinolones
- Trimethoprim - sulfamethoxazole
- Antifungal
- Antihypertensive
Immunosuppressive medications
- Biologics
- Anti-tumour necrosis factor
- Calcineurin inhibitors
- Thiopurines
- Azathioprine
- Methotrexate
- Cyclosporine
- Hydroxyurea
- BRAF inhibitors
- Cyclosporine
- Sonic hedgehog inhibitors
- Janus kinase inhibitors
- Phosphodiesterase 5 inhibitors
|
| Previous radiation therapy1 |
Environmental exposure1
- Arsenic exposure
- Polycyclic aromatic hydrocarbons (found in industrial oils and lubricants)
- Pesticides
- Herbicides
|
Case continued
Two years earlier, the patient had developed myelofibrosis and was treated with 10 mg ruxolitinib twice daily. Her six-week postoperative review appointment was missed as she was admitted for severe anaemia and renal failure. These intercurrent health issues resulted in cancellation of two further appointments.
Twelve weeks postoperatively, she developed a recurrent lesion on the left thumb. Other sites were clear. Urgent excision with a full-thickness skin graft and splinting was performed. Thrombocytopenia resulted in significant intraoperative bleeding.
Histopathology revealed moderately differentiated SCC with an infiltrative growth pattern extending from dermis into the subcutaneous tissue. The tumour’s proximity to the deep margin was 0.5 mm at the centre and within 1 mm over a 5-mm diameter area, with no lymphovascular or neural involvement. After multiple levels, the reporting pathologist was satisfied that the deep margin was close but clear. Further management options discussed included re-excision, radiation therapy or close observation.1
Question 4
What is ruxolitinib?
Answer 4
Ruxolitinib, a Janus kinase (JAK) inhibitor, selectively inhibits JAK1 and JAK2 protein kinases on the JAK/STAT pathway. It is Food and Drug Administration (FDA)-approved for myelofibrosis, polycythaemia vera and steroid refractory graft-versus-host disease. It carries a warning of increased non-melanoma skin cancer (NMSC) risk, especially in patients with previous NMSC, or pre-malignant skin lesions. Prior hydroxyurea treatment increases this risk but was not a factor here.7 Emerging data suggest ruxolitinib-treated patients with NMSC might exhibit more aggressive carcinoma behaviour including perineural invasion and metastasis.8
Case continued
The patient returned for a follow-up at six months after the initial presentation and six weeks following close but clear excision of the left thumb SCC. There were no signs of local or regional recurrence observed on the hand, and the nasal and foot lesions had healed satisfactorily (Figure 3). An informed decision was made to monitor the site closely.
During this review, three additional symptomatic, bleeding skin lesions on the left shoulder, right chest and left thigh were treated by curettage and cautery. The patient was about to leave on a long-anticipated cruise and desired immediate management. Histopathology confirmed IEC. She will be reviewed on return.

Figure 3. Lesions at the 6-week follow-up stage. (A) Healed site post full-thickness skin graft at 6 weeks. (B, C) Healed sites post shave, curettage and cautery at 6 months after initial presentation.
Question 5
How should this patient be managed going forward?
Answer 5
This case demonstrates the increased keratinocyte malignancy risks in patients who are on immunosuppressive medications such as ruxolitinib.9 The patient’s repeated and prolonged admissions for her haematological issues significantly impacted her skin cancer management. The initial procedure with shave and curettage treated two out of three lesions definitively. By addressing the lesions promptly, time that would have been needed with additional procedures to manage the patient’s skin cancers was saved, which is especially important given her increased risk of complications from myelofibrosis.
When planning surgeries for optimal management, it is vital to consider potential delays, especially in complex medical scenarios such as this.
Ongoing management strategies are outlined in Box 1.
| Box 1. Managing non-melanoma skin cancers in immunosuppressed patients |
|
1. Conduct more frequent skin examinations10 and aim to address multiple skin lesions during the same appointment whenever possible.
2. Patients should:
- limit sun exposure
- adopt sun-protective measures
- perform regular self-skin examinations
- be educated about recognising early signs of skin malignancies
- be encouraged to re-present to healthcare professionals (eg general practitioner, dermatology, skin cancer doctor) if concerned.9
3. Use pre-emptive field treatments of solar keratosis to reduce SCC development such as:1,9
- oral chemoprevention with vitamin B3 or acitretin
- topical 5-fluorouracil
- photodynamic therapy
- laser
- chemical peels
- use of volume-modulated arc therapy to treat areas of significant field cancerisation. This would need a careful analysis of risk and benefit.
4. Manage immunosuppressive medication by:
- maintaining patients on the lowest effective dose for better long-term treatment outcomes10
- frequently review medication dosage by the prescribing specialist
- considering alternative medications with less skin cancer risk.11
5. Where SCCs cannot be treated with surgery or radiation, combining cemiplimab, an immune checkpoint inhibitor, with ruxolitinib could synergistically manage skin malignancies while maintaining stability in myelofibrosis.12
6. Multidisciplinary approach9 involving dermatology, plastic surgery, radiation oncology and a general practitioner is vital to ensure optimal treatment outcome while balancing the risks and benefits of immunosuppressive medication in the patient’s situation.
|
| SCC, squamous cell carcinoma. |
Key points
- Clinicians should be alert to factors contributing to increased non-melanoma skin cancers.
- To mitigate skin cancer risks, consider optimising immunosuppressive medication by maintaining the lowest effective dose, undergoing regular dose reviews and consider alternative medications with lower skin cancer risks.
- Addressing multiple lesions in a single visit for co-morbid patients prone to rapid development of multiple skin cancers is critical, due to risk of treatment delays, which require flexible management strategies to adapt to unforeseen challenges.