Popular diets and dietary advice come and go. Some of these perennial common diets promote weight loss; some could be considered specific medical nutrition therapy, whereas others promote non-specific health benefits.
In 2011–12, 13% of Australians aged 15 years and over reported being on a diet for weight loss or other health reasons.1
Primary healthcare professionals should be aware of popular diets and their potential risks and benefits (Figure 1). General practitioners (GPs) can minimise patient harm and direct patients to evidence-based alternatives.2
Below is a commentary on four popular diets highlighting potential considerations, advantages and disadvantages.
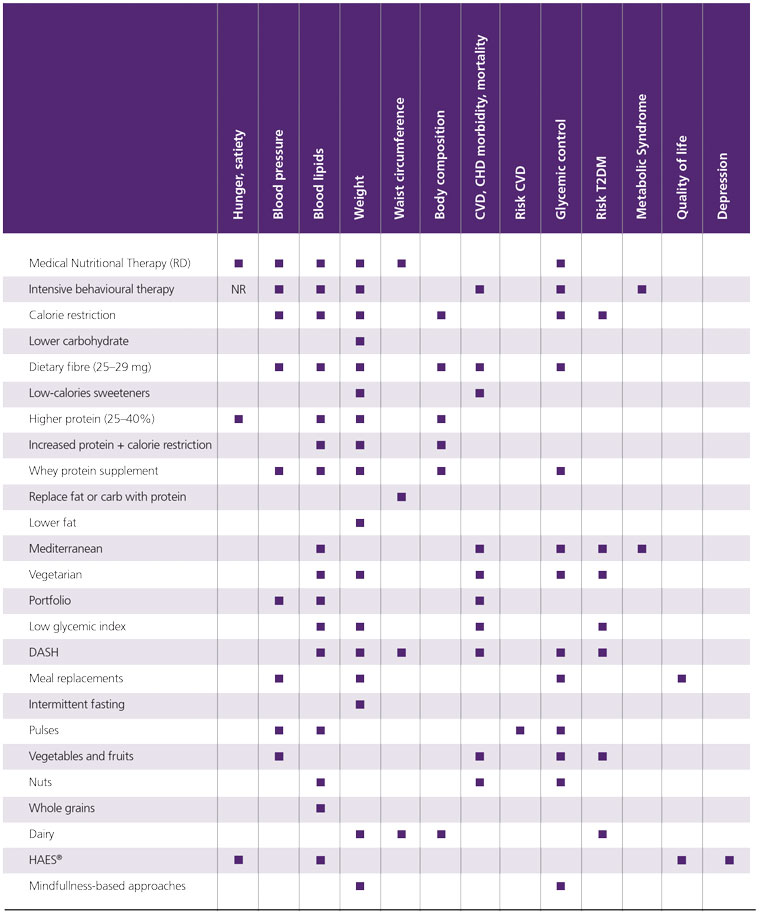
Figure 1. Summary of the clinical outcomes for nutrition interventions.
Reproduced from Obesity Canada. Medical nutrition therapy in obesity management (version 2). Obesity Canada, 2022. Available at https://obesitycanada.ca, with permission from Obesity Canada.
CHD, coronary heart disease; CVD, cardiovascular disease; DASH, dietary approaches to stop hypertension; HAES®, Health at Every Size; NR, not recorded; RD, registered dietitian; T2DM, type 2 diabetes mellitus.
Ketogenic diets
Ketogenic diets have been used for over 100 years.3 Initially used as a therapy to control epilepsy, they are increasingly common in the treatment of type 2 diabetes and/or weight loss.4
Definition
A ketogenic diet induces physiological ketosis via significant carbohydrate intake restriction.
During carbohydrate restriction, the body breaks down stored carbohydrates in glycogen reserves and makes glucose via the liver. At the same time, energy requirements are met through the release of free fatty acids from adipose tissue.
There is no clear definition of a ketogenic diet; however, most ketogenic diets limit total carbohydrate intake to less than 50 g daily.5
Who uses a ketogenic diet?
People who use a ketogenic diet can include:
- those seeking weight loss6
- professional endurance sports athletes
- professional athletes who need to lose weight to meet their weight category or bodybuilders who are preparing for competitions7
- those seeking to improve their blood glucose control.
Ketone bodies can suppress appetite, leading to decreased total energy consumption. Ketogenic diets show greater weight loss at 3–6 months compared to low-fat diets, but the difference disappears at 12 months.6
Ketogenic diets have been shown to positively affect blood pressure, high-density lipoprotein cholesterol, triglycerides, blood glucose, glycated haemoglobin (HbA1C), insulin and C-reactive protein.8
However, some studies have shown an increase in low-density lipoprotein (LDL) cholesterol compared to participants following a low-fat diet. This has led to some healthcare professionals being concerned about an increased risk for the development of atherosclerosis.9 It appears that the ketogenic diet’s effect on LDL cholesterol is nuanced. Ketogenic diets have been reported to increase the size and volume of the LDL cholesterol particles, which is considered to reduce cardiovascular risk as it is the smaller LDLs that are associated with atherogenesis.10 There is a lack of robust evidence regarding the implications of these observed effects on cardiovascular health end points over time.11
Side effects
The side effects of a ketogenic diet include:
- constipation
- ketone breath
- initial dehydration, headaches, nausea and dizziness
- increased risk of kidney stones
- potential for nutrient deficiencies such as B vitamins, vitamin C, potassium, magnesium, fibre and prebiotics.
Potential concerns
Research has shown that long-term compliance with a ketogenic diet is poor.11,12
Adequate dietary fibre, resistant starch and prebiotics can be challenging to achieve, and there are concerns regarding their long-term effects on bowel health and the gut microbiome.
Children and people with liver failure, pancreatitis and inborn fat digestion disorders should avoid this diet. Pregnant and lactating women and those with type 1 diabetes would be best advised not to follow this eating pattern without specific intent, medical monitoring and an understanding of the potential significant risks.
Ketogenic diets should be avoided or used with caution for people using a sodium glucose transporter type-2 inhibitor (SGLT2i) medication. Pathological increases in blood pH via excess ketone bodies can occur in this clinical scenario, even without significantly low blood glucose; this is known as euglycaemic ketoacidosis.13
Low-carbohydrate diet
Definition
Low-carbohydrate diets typically involve a daily carbohydrate intake of less than 100–130 g and/or less than 20–30% of total daily calories.
In comparison, the average Australian diet has more than 250 g of carbohydrate daily and/or more than 55% of total dietary energy from carbohydrates.
Who uses a low-carbohydrate diet?
People who use a low-carbohydrate diet include those seeking:
- weight loss
- improved blood glucose control
- improved cardiovascular health and/or longevity.
The American Diabetes Association and Australian Diabetes Society now accept low-carbohydrate eating as a medical nutrition option for people with type 2 diabetes.14–16 However, it should be noted that the current guidelines recommend individualised personal nutrition therapy, preferably from a registered nutrition professional, and in accordance with the Australian Dietary Guidelines.16–18
Low-carbohydrate diets improve triglycerides and LDL cholesterol, but some people’s genetics might lead to a more atherogenic lipid profile.19
High-level evidence-based conclusions regarding low-carbohydrate eating lack coherent, congruent advice due to heterogeneity among different low-carbohydrate research studies.20
A 2022 Cochrane review compared low-carbohydrate versus balanced-carbohydrate diets for reducing weight and cardiovascular risk and found, with moderate confidence, little to no significant difference in weight loss and diastolic blood pressure, Hb1AC and LDL cholesterol out to two years.21
Potential side effects
The potential side effects of a low-carbohydrate diet include:
Time-restricted eating/intermittent fasting
Definition
Time-restricted eating (TRE)/intermittent fasting (IF) is an eating pattern that limits the time range for consuming calories, including prolonged or modified fasting.
Short-term formal fasting has been a part of human culture for centuries in connection with religious observances.
The current popular TRE/IF diets include:
- 16 : 8 (16 hours fasting, 8 hours eating window; eg eating only between 10 am and 6 pm)
- The 5 : 2 diet (a modified fast on two days)
- Alternate day fasting (ADF). Alternative days of normal eating with days of significantly reduced calorie intake or complete fasting.
What a person eats during their eating window is not defined, and there is a considerable difference in what is considered fasting.
Some suggest restricting the eating window and eating at certain times of the day has favourable metabolic effects. This might be part of the mechanisms of health benefits.22
Proponents of this diet believe that TRE/IF might be a more sustainable approach to weight loss and any of the health benefit claims for many people, as there is no active focus on calorie restriction.
Who uses a TRE/IF eating pattern?
People who use a TRE/IF diet include those:
- seeking weight loss (TRE can reduce energy intake by 10–30% from baseline23)
- seeking improved insulin function and/or blood glucose control
- improved cardiovascular health markers such as decreases in blood pressure, LDL cholesterol and triglyceride levels
- seeking possible favourable changes in the diversity of the gut microbiome
- wishing to increase their longevity (possible effects on telomeres and mitochondrial function).
Fasting might have potential health benefits such as decreasing blood pressure, insulin resistance and oxidative stress. Although findings are variable, it can also lower LDL cholesterol and triglyceride levels.23
There might be favourable changes in the diversity of the gut microbiome, but the evidence is limited.24
To date, studies have been small and of short duration, and longer-term research is needed to understand the sustainable role of intermittent fasting on health.
Potential concerns
In a recent systematic review, intermittent fasting trials reported no serious adverse effects.25
Fasting-related safety concerns include mood-related side effects and binge eating. Study participants occasionally reported dizziness, weakness, bad breath, headache, feeling cold, lack of concentration, sleep disturbance, nausea and constipation. Whether they were significantly different from the baseline has been challenged in other studies.
Fasting is not recommended for pregnant or lactating women or individuals with a history of eating disorders. It is also not appropriate for those who need to take medication with food at specific times during the day.
Mediterranean diet
Definition
The Mediterranean diet is a traditional eating pattern that originated in the Mediterranean basin during the 1950s and 1960s.
What constitutes a Mediterranean diet is not strictly defined,26 but several scoring assessments can evaluate an individual’s alignment with this eating pattern.27,28
The Mediterranean diet is a flexible pattern with such variability that it has led to inconsistencies in definitions and assessment.26 However, compared to a typical Western diet, the Mediterranean diet has less red meat, processed meats, more fish and a greater emphasis on fresh fruits and vegetables, whole grains and monounsaturated fats such as olive oil, avocado and nuts.29
One of the distinguishing features of this diet is its relatively low intake of added sugars and refined carbohydrates.
This is in contrast to the current Australian eating pattern, where more than 30% of energy intake is from discretionary foods.30 Examples of discretionary foods include biscuits, confectionery, pastries, processed meats, salty snack foods and sugar-sweetened beverages. Discretionary foods are typically low in essential nutrients and high in energy, saturated fat, added sugar and/or added salt.
Specifically, a Mediterranean diet has a:
- high monounsaturated/saturated fat ratio (use of olive oil as a main cooking ingredient)
- high consumption of vegetables, fruits, legumes, whole grains
- and cereals
- moderate consumption of dairy and poultry products
- low-to-moderate consumption of
- red wine
- low consumption of meat and meat products
- increased consumption of fish.
Who uses a Mediterranean diet?
There is good evidence that following a Mediterranean diet can help with the following chronic health conditions:31
- cardiovascular disease
- obesity
- cognitive function
- some cancer risks
- mental health
- insulin resistance and its associated health conditions such as prediabetes/type 2 diabetes/metabolic syndrome.
Evidence is based on both population studies (eg Seven countries study by Keys et al,32 Lyon Diet Heart study by de Lorgeril et al33) and intervention studies (eg Prevención-con-Dieta-Mediterránea [PREDIMED] by Krone et al34).
Potential concerns
Some of the potential health advantages seen in observational studies might be due to lifestyle factors (such as increased socialisation and physical activity) rather than singular nutrients or foods alone.
The Mediterranean diet is very different from typical Australian eating patterns,35,36 and often, an individual’s interpretation does not correlate with the accepted definition of Mediterranean-style eating.26
Food for thought
Evidence-based dietary advice is best; however, an individual’s interpretation and implementation of specific diets can be wildly individual, and long-term adherence can be challenging.
My advice to patients is that the best diet for them is one that uniquely meets their individual health priorities, is one they can adhere to for the rest of their lives and is considered nutritionally healthy.37
An alternative to following a popular singularly restrictive diet is the Australian Dietary Guidelines (under review); however, it should be noted that most Australians do not meet the current recommendations.38
The following is a helpful resource for empowering patients to apply critical thinking regarding non-specific dietary advice: Evaluating-Dietary-Advice