Feature
October–December 2020: Emerging from the darkness
The final months of the year have been a time of transition, progress, solidarity and hope for general practice in Australia.
 The final months of 2020 have presented something of a rollercoaster for general practice in Australia.
The final months of 2020 have presented something of a rollercoaster for general practice in Australia.
As Australia moved out of the depths of winter and began to get a grip on the coronavirus crisis that had threatened to sweep across Victoria, attention turned to how the rest of the world was coping with the deadly disease.
Reports of a falling death rate had some questioning whether harsh restrictions were the correct approach, before a global resurgence reinforced the success of Australia’s containment strategy.
The first week of October was also a time of great uncertainty, after it was revealed US President Donald Trump had contracted COVID-19.
While there were initial concerns as to how the 74-year-old would cope with the disease, they soon transitioned into curiosity after he made a full recovery, thanks in part to the ‘investigational antibody cocktail’ REGN-COV2.
Early October also saw GPs stand up and defend their profession, as news broke of a South Australian public servant asking public hospital surgeons to ‘say no’ to GP referrals for ‘old’ patients or those with comorbidities.
The controversy provoked a strong response from RACGP Acting President Associate Professor Ayman Shenouda, who pointed out that GPs are more than capable of managing the care of older patients – particularly those with complex comorbidities – and that it was highly inappropriate for public servants with no clinical experience to second-guess primary care specialists.
‘GPs have the skills and knowledge to analyse and manage the vast majority of conditions our patients face. We do this every day,’ he told newsGP at the time.
‘We know our patients better than any other health professional and should be trusted to help them make choices that represent the high-quality care Australians expect from their GP.’
However, despite the show of solidarity, it was not long before GPs were once again forced to defend their expertise – albeit in very different circumstances.
The first challenge came in the form of an offensive question from a dad in a local park, which many GPs saw as indicative of the dismissive attitude some people still hold towards general practice.
‘You’re just a GP … aren’t you?’, the man asked Melbourne GP Dr Claire Denness after she had spent the past three months on the coronavirus frontline.
While she did not respond at the time, Dr Denness’ subsequent column in newsGP drew an impassioned response from the general practice community as GPs across the country shared their own experiences in solidarity.
The second challenge was much more high profile, offensive and personal.
Former celebrity chef Pete Evans, who has regularly drawn the ire of doctors around the country by making dangerous and ill-considered comments on numerous health issues, took it a step further when he suggested recently deceased RACGP President Dr Harry Nespolon had passed away because he did not know how to properly treat his own pancreatic cancer.
The comments, made during a Facebook Live interview, provoked a ferocious response from GPs, the wider medical community and the general public, as people stood up to defend the reputation of a doctor who had continued to dedicate his life to his patients and the betterment of general practice until the end.
October was also a difficult month for many future GPs, as an unprecedented technical issue resulted in more than 1400 candidates not being able to complete their Key Feature Problem (KFP) exam and Applied Knowledge Test (AKT).
While the college swiftly apologised and moved quickly to compensate those affected, the failure was devastating for many and upsetting for all involved. RACGP CEO Dr Matthew Miles addressed the controversy in a Q&A with members, in which he expressed the college’s ‘deep regret’ over having to cancel the exams, and explained what the RACGP had done and continues to do to help affected candidates.
The first KFP and AKT re-sits progressed without issue.
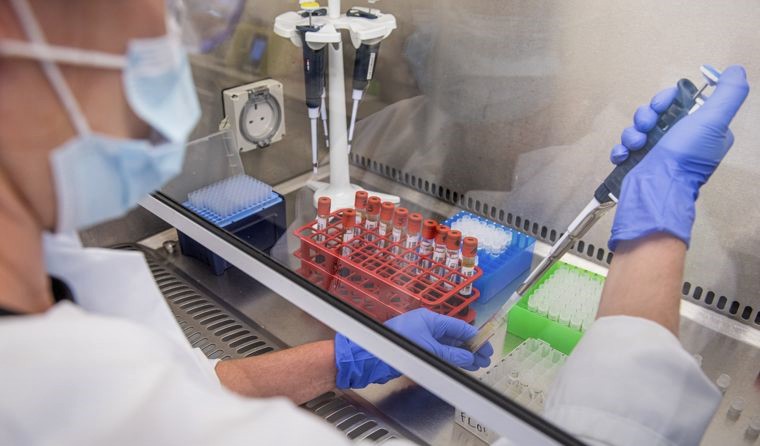
The global race for a successful COVID vaccine has been a key feature of the final months of 2020. (Image: AAP)
November brought with it the traditional Medicare Benefits Schedule (MBS) update, before news of the impending coronavirus vaccine rollout turned people’s attention to ongoing clinical trials of the most advanced candidates, including those that have never before been widely given to humans.
A major focus on the clinical trial process – including temporary pauses and in some cases outright abandonment – has prompted concerns regarding vaccine hesitancy, with GPs likely to play a major role in assuaging the fears of the general public.
In another ground breaking moment stemming from the unique circumstances generated by the coronavirus pandemic, the RACGP’s annual conference took place entirely online for the first time ever.
GP20 delivered a mix of on-demand and live sessions across a range of clinical and professional topics, including business of general practice, addiction medicine, and how racism is a public health crisis that cannot be ignored.
The success of the conference was followed by more good news for general practice, when the Federal Government announced the permanent extension of universal access to telehealth on 27 November.
Associate Professor Shenouda welcomed the commitment, describing it as a ‘fundamental building block of primary healthcare reform’.
‘GPs and patients have benefited significantly from telehealth services and we have been actively lobbying the [Federal] Government to see them become a permanent fixture,’ he said.
‘While we are keen to see the details of a long-term, permanent telehealth plan … [GPs] can now look forward to permanent Medicare subsidies allowing them to continue offering these services.’
Shortly after the permanent extension was announced, Dr Karen Price officially began her term as RACGP President, with RACGP Queensland Chair Dr Bruce Willett named as Vice-President.
Upon assuming the role, Dr Price spoke of her ‘extraordinary faith’ in the RACGP’s community of members and reinforced her ‘firm belief’ that teamwork and coordination drive outcomes.
Writing exclusively in newsGP, Dr Price set out the priorities for her two-year term and urged everyone to play a role in creating a stronger primary care system.
GPs received another welcome dose of positive news in the final month of 2020, after it was revealed their role in helping patients navigate the National Disability Insurance Scheme is close to finally being defined, while ‘huge advances’ in the diagnosis and management of iron deficiency led to new clinical guidance.
Additionally, Australia topped an international healthcare survey in which access to primary care and trust in domestic healthcare services were rated extremely highly; the RACGP released a well-received interactive MBS tool that was ‘just what the doctor ordered’; and the college appointed its first ever Aboriginal Censor.
In the final weeks of 2020, new modelling from PwC Australia confirmed the billions in savings and advances in quality of life greater investment in primary care could achieve, and Dr Cathy Andronis was awarded a seat on the Mental Health Australia Board.
The MBS Review Taskforce also handed down its final report, after trawling through and evaluating in excess of 5700 MBS items over the past five years. It recommended more than 1400 changes, including more use of block or blended payment models rather than fee-for-service funding.
At the time of publication, the Federal Government had accepted 520 of the recommendations.
Log in below to join the conversation.
coronavirus COVID-19 pandemic RACGP
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?