Approximately one million Australians have diabetes mellitus (DM), with estimates projected to rise to three million by 2025.1 In 2014, 1 per 100 women giving birth in Australia had pre-existing DM.2 Women with diabetes have higher incidences of maternal, fetal and neonatal complications, including increased risk of congenital anomalies.3 Many of these risks can be reduced through tight glycaemic control before and during pregnancy.4 International5 and Australian guidelines6 recommend at least annual preconception counselling for all women of reproductive age who have DM. Despite this, most international studies and the one national audit report that only 30–40% of women with DM seek preconception care (PCC) and plan the timing of their pregnancies.7,8
One major barrier to pregnancy planning is access to, and use of, reliable contraception. Although nearly 70% of Australian women of child-bearing age report using contraception,9 38.8% of women who had previously been pregnant reported a previous unintended pregnancy.10 On the basis of overseas data, approximately half of these unintended pregnancies result from inconsistent or incorrect use of contraception.11 Large studies show that unplanned pregnancies can be reduced through employment of less user-dependent methods of contraception, particularly the most reliable reversible methods – the long‑acting reversible contraceptives (LARC), including contraceptive implants and intrauterine contraception (IUC).12 IUC methods available in Australia are the copper intrauterine devices and the levonorgestrel intrauterine system.
There are few studies exploring pregnancy planning and contraceptive use in Australian women with DM.13,14 To our knowledge, there are no Australian studies in women with DM exploring their use of contraception, nor their beliefs regarding the safety of different methods. Among a cohort of women with DM, the aim of this study was to explore women’s understanding of the importance of pregnancy planning and the implications of poor glycaemic control on pregnancy outcomes, beliefs regarding the safety of different contraceptive methods in DM, sources of contraception information and contraception use.
Methods
We undertook a quantitative cross-sectional questionnaire-based study in the Nepean Blue Mountains Local Health District (NBMLHD), a large tertiary referral centre. Between August 2013 and August 2015, we approached eligible women of reproductive age (16–49 years) with DM (type 1 or 2) to participate in the study. Women attending the diabetes service were invited at their scheduled clinic appointment or via mail/email to complete the survey. Women were sent a letter explaining the purpose of the survey, a plain language information flyer, a consent form and a paper copy of the survey. A reminder letter was sent three weeks later. The survey was promoted via local media and flyers displayed in the hospital.
The self-administered survey was available online or as a written postal survey. Survey questions were based on diabetes and pregnancy guidelines,7 the findings from a literature review and consultation with experts in pregnancy and diabetes. The survey (available online only) comprised 22 questions addressing demographic information (seven questions), thoughts and beliefs regarding pregnancy and contraception in DM (nine questions), current contraceptive practice (four questions) and previous pregnancies (two questions). Pilot testing was conducted with five women to optimise survey question clarity.
Participants were assigned a study number, and results were de-identified to maintain confidentiality. The data were analysed using SAS version 9.4. Any instances in which responses to a particular question were missing were noted (supplementary table, available online only), and the percentages were calculated using the number of women who answered that question as the denominator.
Chi-square tests were used to determine whether there were significant differences between categorical demographic characteristics and participants’ responses to questionnaire questions. This was performed as a post-hoc analysis for four participant characteristics.
The study was approved by the NBMLHD Human Research Ethics Committee.
Results
A total of 107 of 215 women participated in the study, a response rate of 49.8%. Several questions had missing responses (
<5 per question). The mean age of participants was 26.7 years (range 16–49 years). The majority had type 1 DM (79.4%) and were Australian-born (89.6%). Other participant characteristics are shown in Table 1.
| Table 1. Characteristics of women who completed the survey (n = 107) |
| |
n (%) |
| Type of diabetes |
|
| Type 1 |
85 (79.4) |
| Type 2 |
17 (15.9) |
| Not sure |
5 (4.7) |
| Duration of diabetes* |
|
| <1 year |
9 (8.4) |
| 1–5 years |
25 (23.4) |
| 6–10 years |
16 (14.9) |
| >10 years |
57 (53.3) |
| Age group |
|
| 16–24 years |
51 (47.7) |
| 25–34 years |
39 (36.4) |
| 35–44 years |
14 (13.1) |
| 45–49 years |
3 (2.8) |
| Country of birth |
|
| Australia |
95 (89.6) |
| Other |
11 (10.4) |
| Current relationship status |
|
| Single |
36 (33.6) |
| In a relationship |
29 (27.1) |
| Married or de facto |
39 (36.4) |
| Widowed |
1 (0.9) |
| Divorced/separated |
2 (1.8) |
| Highest level of education completed (n = 106) |
|
| Primary school† |
10 (9.4) |
| High school‡ |
48 (44.9) |
| TAFE/university course |
48 (44.8) |
| Employment§ |
|
| Studying full time |
23 (21.5) |
| Studying part time |
10 (9.4) |
| Working full time |
37 (34.6) |
| Working part time |
26 (24.4) |
| Unemployed |
15 (14.0) |
| Pension |
10 (9.3) |
| Sexually active |
|
| Yes |
87 (81.3) |
| No |
20 (18.7) |
*Duration of diabetes was determined by current age minus age at diagnosis of diabetes
†Includes six women currently at high school
‡Includes 17 people who have attended high school to at least the level of Year 10
§14 women reported both working and studying |
The responses to questions about pregnancy planning and contraception are documented in Table 2, including a comparison between answers of women with types 1 and 2 DM. Most women (83.4%, n = 86) were aware of potential maternal and fetal complications associated with DM in pregnancy, while half (50.5%, n = 52) were unsure of the need for medication changes prior to or during pregnancy. Contraceptive choice was regarded by most (61.2%; n = 63) not to be significantly limited by DM. Over three quarters (77.7% = 80) believed combined oral contraceptive pills (COCPs) were safe in DM. However, 61.7% (n = 66) were unsure of the safety of IUC in DM, and 43.7% (n = 45) were unsure about the safety of contraceptive implants (Figure 1). Excluding women who were unsure of their diabetes type (n = 5), understanding of the complications and need for medication change was not different between those with types 1 and 2 DM. Women with a TAFE qualification or university degree were more likely to be aware of potential complications associated with DM in pregnancy than those whose highest level of education was secondary education: 93.7% of women, compared with 67.5% (P = 0.0021). They were also more likely to know that they might need medication changes prior to pregnancy: 40% of women, compared with 25% (P = 0.0181).
| Table 2. Participant responses to questions about pregnancy planning and contraception among reproductive age women (n = 103) with comparison of pattern of answers between women with type 1 and type 2 diabetes mellitus (n = 98)* |
| |
Overall
n (%) |
Type 1 diabetes mellitus
n (%) |
Type 2 diabetes mellitus
n (%) |
P value |
Have you ever discussed pregnancy planning during visits with your general practitioner or endocrinologist?
Yes
No |
29 (28.2)
74 (71.8) |
22 (27.2)
59 (72.8) |
7 (41.2)
10 (58.8) |
0.25 |
Do you know if you need to stop or change medication before or during pregnancy?
Yes
No
Not sure |
35 (34.0)
16 (15.5)
52 (50.5) |
27 (33.3)
15 (18.5)
39 (48.2) |
7 (41.2)
1 (5.9)
9 (52.9) |
0.43 |
Do you think there are potential complications or health problems associated with diabetes in pregnancy for you or the baby?
Yes
No
Not sure |
86 (83.5)
3 (2.9)
14 (13.6) |
67 (82.7)
1 (1.2)
13 (16.1) |
16 (94.1)
1 (5.9)
0 (0) |
0.0695† |
Do you think women with diabetes have more limited contraceptive choices?
Not/minimal limits
Don’t know
Quite/very limited |
63 (61.2)
34 (33.0)
6 (5.8) |
53 (65.4)
25 (30.9)
3 (3.7) |
7 (41.2)
8 (47.1)
2 (11.8) |
0.0963† |
*Excluding women who were unsure of diabetes type (n = 5) and those with missing data, who all had type 1 diabetes mellitus (n = 4)
†Fisher’s exact test was used in place of chi-square test where a number of cell counts were less than 5 |
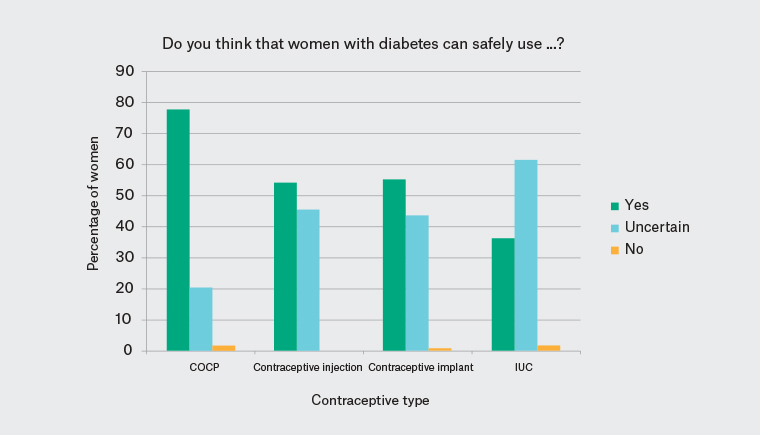
Figure 1. Contraceptive knowledge of the safety of different methods in women with diabetes
COCP, combined oral contraceptive pill; IUC, intrauterine contraception
For 69.9% (n = 71) of the participants, the general practitioner (GP) was the main source of information regarding contraception, followed by school (35.3%, n = 36) and family (29.4%, n = 30). Endocrinologists (15.7%, n = 16) and diabetes educators (14.7%, n = 15) were uncommon sources.
Of the 87 women (81.3%) who had ever been sexually active, 46 (54.8%) reported a previous pregnancy and one reported a current pregnancy. Of these, 40 had at least one live birth (parity range 1–7), 16 had at least one miscarriage (range 1–4 with a total of 32 miscarriages) and four had one or more stillbirths (total of seven stillbirths). There were 12 terminations of pregnancy in 10 women.
Only 28.2% of women had ever had a specific discussion around planning for a pregnancy with their endocrinologist or GP. Even among sexually active women, approximately two-thirds (65.5%, n = 57) had never had a specific discussion around planning for pregnancy. Of the 47 women who had been or were currently pregnant, preconception advice was reported by less than half (46.8%, n = 22).
Of the 87 women who had ever been sexually active, condoms were the most commonly used form of contraception (87.2%, n = 75), followed by COCPs (74.4%, n = 64), contraceptive implants (18.6%; n = 16), contraceptive injections (14.0%, n = 12), IUC (4.6%, n = 4), female sterilisation (2.3%, n = 2) and male sterilisation (2.3%, n = 2). Sixteen per cent (n = 14) of sexually active women had never used any form of contraception. Contraception use in the last 12 months is documented in Table 3. Almost a quarter of the women (24.7%, n = 21) reported no use of contraception, and only three (3.5%) were using one of the LARC methods.
| Table 3. Main contraception used in the last 12 months among ever sexually active women (n = 85) |
| Contraceptive method |
Number (%) |
| Nil |
21 (24.7) |
| Condoms |
18 (21.2) |
| Combined oral contraceptive pill (COCP) |
17 (20.0) |
| Intrauterine contraception |
0 (0) |
| Injection |
3 (3.5) |
| Implant |
6 (7.0) |
| Female sterilisation |
1 (1.2) |
| Male sterilisation |
2 (2.4) |
| Not applicable (one specified no intercourse) |
2 (2.4) |
| Other (one breastfeeding, one withdrawal) |
2 (2.4) |
| Multiple methods: condoms plus COCP |
6 (7.0) |
| Multiple methods: nil ± condoms and pregnant |
3 (3.5) |
| Multiple methods: other |
4 (4.7) |
Discussion
This study found that despite knowledge of the adverse effects of DM on pregnancy, Australian women with DM report low rates of preconception counselling and care. Optimal pregnancy planning requires use of reliable contraception, but women in this study expressed uncertainty about the most reliable methods – IUC and implants. Of concern, many of the sexually active women in the study were not using any method or were not using the most reliable methods.
Reported rates of preconception counselling among all women with DM were exceptionally low at 28.2% in our study. In a 2015 National Diabetes Services Scheme (NDSS) survey of 967 Australian women with DM,13 70% reported discussion with a health professional regarding pregnancy, although this was markedly lower in women with type 2 DM (44%). In that survey, the majority of pregnancy-related conversations with a health professional were initiated by the patient (59%). A number of factors may have contributed to the differences in rates between these two studies, including a low response rate for the NDSS survey (16%), potential response bias in that women who had received preconception counselling or who had better knowledge of pre-pregnancy planning may have responded to the survey, and the age and education level of the respondents. Our sample was younger (mean age of 26.7 years in our study, compared with 34 years for NDSS), less educated and of lower socioeconomic status than the NDSS patient population, which likely has an impact on the understanding and experience of DM-related pregnancy risks.
Our findings are also significantly worse than those reported in France15 and the UK,16 where rates of preconception counselling occurred for 85% of women with type 1 DM and 67% of women with type 2 DM, but similar to those in a US study of 80 women with type 1 DM, in which 65% indicated no knowledge of PCC.17 Although not seen in our study, which had low numbers of women with type 2 DM, other studies show that women with type 2 DM are at particular risk of being overlooked for preconception counselling. These women more often receive non-specialist care, have associated obesity and metabolic syndrome (which confer high risks for pregnancy) and are at risk of continuing potentially teratogenic medications (eg statins).18 This is particularly an issue for Aboriginal and Torres Strait Islander mothers, who have a 10 times greater rate of type 2 DM compared with the general maternal population, and higher rates of adverse perinatal outcomes.19
Consistent with previous Australian studies,9,20 the forms of contraception most commonly used by women of reproductive age were condoms and COCPs. Reported use of the most reliable methods – the LARC methods – was higher for implants but lower for IUCs when compared with national rates,9 and lower than international rates for both implants and IUCs.21 One study has shown that with a clear ‘LARC first’ counselling strategy, over two-thirds of young women under the age of 25 years will choose an IUC method or implant.12 It is particularly important that LARC is considered a first-line option in women with DM, as the risks associated with unplanned pregnancy are high. Furthermore, even in women with nephropathy, retinopathy, neuropathy or other vascular disease, the implants and IUC are not contraindicated, unlike COCPs.22 However, misconceptions regarding safety and side effects in both patients and providers, lack of training in LARC insertion and poor awareness of LARC benefits contribute to low uptake in Australia.23,24
The main source of contraceptive advice identified in our study was GPs, while discussions with endocrinologists or diabetes educators were uncommon. Therefore, GPs have a crucial role to play in alleviating uncertainty about the LARC methods and in contraception provision, while endocrinologists should consider knowledge of contraceptive options for women with DM part of their remit.
The main strength of this study is that it is the first Australian study to provide data on preconception counselling, contraceptive use and knowledge regarding diabetes and pregnancy in women of reproductive age with DM in Western Sydney. Limitations of the study include the small sample size and predominantly young, Australian-born population of lower socioeconomic background, which may limit generalisability of results. The questionnaire format of the study may have led to recall bias, in addition to the potential for fabricated answers because of fear of embarrassment, although questionnaire responses were coded and thus de-identified to minimise the risk of fabricated answers. Results are descriptive and adjustments have not been made for potential confounders in the limited chi-square testing performed.
In conclusion, women of childbearing age with DM in the NBMLHD understand that there are pregnancy-related risks in DM but have limited uptake of preconception planning. Although LARC methods are recommended in clinical guidelines, women with DM have substantial uncertainty regarding their safety in DM. Use of contraceptive implants is higher than national averages, but reported IUC use is lower. Health professionals, particularly GPs and endocrinologists, need to be proactive in initiating conversations around pregnancy planning and revisiting the topic yearly, including providing advice on safe, effective forms of contraception to avoid unintended pregnancy. Employment of the ‘One Key Question’ initiative, asking ‘Would you like to become pregnant in the next year?’, is recommended.25 However, even when the response is ‘no’, it is prudent to discuss both preconception planning and contraception, as a high proportion of pregnancies are unplanned.
| Supplementary table. Number of responses and number of missing values for each question in contraception questionnaire |
| Question |
No. of participants who answered |
No. of participants eligible to answer |
No. of missing values |
| 1. Age |
107 |
107 |
0 |
| 2. Country of birth |
106 |
107 |
1 |
| 3. Relationship status |
107 |
107 |
0 |
| 4. Age of diagnosis of diabetes mellitus |
107 |
107 |
0 |
| 5. Type of diabetes mellitus |
107 |
107 |
0 |
| 6. Level of education |
106 |
107 |
1 |
| 7. Current employment status |
107 |
107 |
0 |
| 8. Sources of knowledge regarding contraception |
102 |
107 |
5 |
| 9. Specific discussion around pregnancy with general practitioner/endocrinologist |
103 |
107 |
4 |
| 10. Knowledge of whether medications need to be changed prior to or during pregnancy |
103 |
107 |
4 |
| 11. Do you think there are potential health problems associated with diabetes mellitus in pregnancy? |
103 |
107 |
4 |
| 12. Do you think women with diabetes mellitus have more limited choices of contraception than those without diabetes mellitus? |
103 |
107 |
4 |
| 13. Do you believe that women with diabetes mellitus can safely take the oral contraceptive pill? |
103 |
107 |
4 |
| 14. Do you think that women with diabetes mellitus can safely use a contraceptive implant? |
103 |
107 |
4 |
| 15. Do you think that women with diabetes mellitus can safely use the contraceptive injection? |
107 |
107 |
0 |
| 16. Do you think that women with diabetes mellitus can safely use an intrauterine device? |
107 |
107 |
0 |
| 17. Have you ever been sexually active? |
107 |
107 |
0 |
| 18. What forms of contraception have you ever used? |
86 |
87 |
1 |
| 19. What has been your main form of contraception in the past 12 months? |
85 |
87 |
2 |
| 20. What has been your main form of contraception in the past month? |
84 |
87 |
3 |
| 21. Have you ever been pregnant? |
84 |
87 |
3 |
| 22. If you have been pregnant, how many times have you had each of the following? (Live birth, stillbirth, miscarriage, termination of pregnancy, ectopic pregnancy) |
46 |
47 |
5 |