Australia was the first country in the world to develop a National Pain Strategy in 2011.1 One of its key goals was improving access to interdisciplinary care, with two key objectives being 1) develop and evaluate patient-centred service delivery and funding models for pain management in the community that provide interdisciplinary assessment, care and support as a part of comprehensive primary healthcare centres; and 2) ensure meaningful communication about pain management between practitioners and patients, and between practitioners. A 2009 survey of Australian pain centres2 had revealed a median wait time of 150 days for publicly funded adult outpatient pain management services.
Primary care pain centres could provide patients with a diagnosis, prognosis and management strategy ‘at one sitting’. However, interdisciplinary spinal pain clinics conducted from primary care are rare in Australia. A search of the literature found no papers reporting on the outcomes of primary care interdisciplinary pain clinics.
With this in mind, in 2011 four practitioners – a physiotherapist, pain and rehabilitation physician, musculoskeletal physician (lead author [SM]) and neurosurgeon – set up a monthly interdisciplinary clinic. The main objective was to enhance interdisciplinary care for patients with complex spinal pain and provide a diagnosis, prognosis and management strategy ‘at one sitting’. The aim of this paper is to report on the evaluation of this community-based clinic.
Methods
We conducted a longitudinal audit of patients attending a single interdisciplinary pain clinic. Approval for the research was granted through the University of Queensland Medical Research Ethics Committee (approval number 2014001622).
Setting
The clinic is based in Caloundra, Queensland, which is categorised as a Modified Monash Model (MMM) 1 region. Patients came largely from the Sunshine Coast district or surrounds with MMM 1–5 classifications. During consultation, each patient met first with the musculoskeletal physician and physiotherapist simultaneously. Their focus was on identifying vertebral and myofascial dysfunction, abnormal movement patterns, gait and proprioceptive abnormalities. Following this, the surgeon and pain and rehabilitation physician met the patient together to identify any red flags or surgical lesions and to determine whether pain intervention procedures were suitable for the patient. Both teams considered the patient’s psychosocial context and a diagnostic framework. Both teams then formulated an individually tailored joint management and referral plan, involving a wide network of private and public services and practitioners including psychologists, psychiatrists, physiotherapists and other medical specialists. The patient (and accompanying persons) were then provided with a diagnosis, and invited to discuss the proposed management plan and decide on future steps with all four practitioners. This joint case conference was designed to provide reinforcement of the same health messages.
In addition, written reports, investigation results and plans were provided to the patient, referring general practitioner (GP) and other involved practitioners within the week. The patient was encouraged to see their referring GP within that month. At least one person of the team also undertook subsequent patient follow-up.
The clinic charged patients an out-of-pocket expense of no more than $400, less for pensioners. Department of Veterans' Affairs (DVA) patients and workers compensation patients were also seen at the clinic.
Participant selection
Twelve clinics were held between August 2012 and September 2014, and 88 patients seen. Each patient needed a referral from their GP. Patients who presented to the clinic during the above two-year period were sent invitations by mail to participate in follow-up evaluation of their progress. Non-repliers received a subsequent phone request. Consent was obtained for participation in the research project through returned written consent or verbal consent over the phone. Participants were excluded if their initial pain and disability questionnaires were not saved on file. Fifteen doctors who referred frequently to the clinic were also mailed invitations to give feedback on the clinic.
Data collection
Initial data were collected from the standard questionnaire provided to all patients presenting to the clinic (Appendix 1; available online only), which includes a modified Brief Pain Inventory (BPI).3 Summated pain scores were calculated by adding the four pain scores together from the BPI. Disability data were derived from the second section of the BPI. Patients rated how pain interfered with seven aspects of life on a 0–10 scale. Summated scores out of 70 were calculated for disability. The BPI is a well-validated tool for use in chronic non-malignant pain.3
Patients’ pain type had also been diagnosed by the team at their first presentation. This was divided into somatic, somatic-referred, radicular or neuropathic. International Association for the Study of Pain definitions were used. Sites of pain were derived from pain body maps. Standard demographic data were also collected.
At follow-up, independent research assistants conducted phone interviews. They used the same modified BPI questionnaire together with patient satisfaction data. This comprised 12 broad questions (Appendix 2; available online only) with a five-point Likert scale and free-text responses. Participants were contacted 2–3 years after their previous clinic visit. Referring doctors gave feedback on their satisfaction with the clinic through seven questions using a five-point Likert scale (Appendix 3; available online only) and free-text responses.
Data analysis
Descriptive statistics (mean and standard deviations) were calculated for pain scores and scores for disability (pain interaction with activity). A paired sample t-test was used to determine differences in summated pain score and summated score for disability between pre-intervention and post-intervention time points.
Significance was set at an alpha value of 0.05 and the precision of estimates reported using a 95% confidence interval (CI). Feedback from the referring doctors was described qualitatively.
Results
Seventy-four of the 88 patients seen during the research period had adequate baseline data, and 44 consented to participate in this study.
Participant characteristics are represented in Table 1. Females predominate (65%) in this cohort, and ages ranged 33–92 years (mean 58 years). The most common pain pattern was somatic lumbar spinal pain with or without referral to the buttock and legs (71%). Somatic referred pain, neuropathic and radicular pain were also common patterns. Mean duration of pain was 51 months, making this cohort a group with very persistent spinal pain.
| Table 1. Patient characteristics |
| Variable |
n |
| Total |
43 |
| Men, n (%) |
15 (35) |
| Women, n (%) |
28 (65) |
| Age (years), mean (SD) [range] |
58.4 (14.5) [33–92] |
| Occupation |
|
| Pensioner |
6 |
| Retired |
7 |
| Physical job |
13 |
| Sedentary job |
11 |
| Student |
1 |
| Not recorded |
4 |
| Pain area, n (%) |
|
| Lumbar |
8 (17) |
| Lumbar/gluteal |
4 (8) |
| Lumbar/gluteal/leg |
22 (46) |
| Cervical |
3 (6) |
| Cervical/shoulder |
2 (4) |
| Cervical/shoulder/arm |
7 (15) |
| Thoracic |
2 (4) |
| Duration of pain (months), mean (SD) |
51 (75) |
| Type of pain, n (%) |
|
| Somatic |
9 (21) |
| Somatic/radicular |
3 (7) |
| Somatic/SR |
13 (31) |
| Somatic/SR/radicular |
2 (5) |
| Somatic/SR/neuropathic |
5 (12) |
| Somatic/neuropathic |
6 (14) |
| Radicular |
4 (10) |
| SD, standard deviation; SR, somatic referred |
The changes in pain scores and disability from initial assessment to follow-up are presented in Figures 1 and 2. The mean summated pain score was 21.0 at presentation and 14.2 at follow-up. The mean difference pre-clinic to post-clinic was −6.8 (95% CI: −3.8, −9.8). The mean summated disability score at presentation was 42.3 and 25.8 at follow-up. The mean difference was −16.5 (95% CI: −9.6, −23.5). Approximately one-half had 30% or more improvement in their summated pain scores, and a similar amount had improvements in disability (effect of pain on activity/mood). Improvements of this amount are considered clinically significant.4 Participants who had improvements in their summated pain and disability scores were more likely to rate their satisfaction with the clinic as positive and feel they were taking more responsibility for their health.
Satisfaction data are shown in Table 2. Participants most commonly agreed with the statement that ‘the health care team working together is important for my overall health’, with two-thirds agreeing or strongly agreeing. Sixty-three per cent of patients agreed or strongly agreed with ‘I was fully satisfied with the service provided’. Forty per cent disagreed or disagreed strongly with ‘the clinic is close to where I live’.
| Table 2. Patient satisfaction responses, n (%) (35 responses, 8 blank) |
| |
Strongly agree |
Agree |
Neutral |
Disagree |
Strongly disagree |
| I was fully satisfied with the service provided by the clinic* |
14 (40.0) |
8 (22.9) |
5 (14.3) |
4 (11.4) |
4 (11.4) |
| The clinic is close to where I live |
5 (14.3) |
10 (28.6) |
3 (8.6) |
10 (28.6) |
7 (20.0) |
| The length of the time spent with the Specialist Team was about right |
10 (28.6) |
15 (42.9) |
3 (8.6) |
5 (14.3) |
2 (5.7) |
| The clinic seemed to be well organised |
7 (20.0) |
21 (60.0) |
3 (8.6) |
4 (11.4) |
0 |
| The cost of the clinic was affordable to me |
4 (11.4) |
19 (54.3) |
5 (14.3) |
3 (8.6) |
4 (11.4) |
| I was given opportunity to ask questions about my care |
8 (22.9) |
18 (51.4) |
3 (8.6) |
4 (11.4) |
2 (5.7) |
| The health care team (specialists, GP, physiotherapists, others) is important for my overall health |
14 (40.0) |
15 (42.9) |
3 (8.6) |
2 (5.7) |
1 (2.9) |
| My use of prescribed pain killers has decreased |
10 (28.6) |
9 (25.7) |
3 (8.6) |
8 (22.9) |
5 (14.3) |
| My use of over-the-counter pain killers has decreased since attending the clinic |
7 (20.0) |
9 (25.7) |
7 (20.0) |
8 (22.9) |
4 (11.4) |
| My overall use of health providers has decreased since attending the clinic |
5 (14.3) |
15 (42.9) |
4 (11.4) |
9 (25.7) |
2 (5.7) |
| I have gained more knowledge about my condition since attending the clinic |
7 (20.0) |
14 (40.0) |
4 (11.4) |
9 (25.7) |
1 (2.9) |
| I am taking more responsibility for my health since attending the clinic |
9 (25.7) |
23 (65.7) |
2 (5.7) |
1 (2.9) |
0 |
|
*Clinic name removed from statements
GP, general practitioner |
Forty-four per cent reported decreased use of prescription analgesics, and 37% reported decreased use of over-the-counter pain relievers. Forty-four per cent reported decreased overall use of health providers. A majority of participants reported feeling more knowledgeable about their condition and taking more responsibility for their health.
A core group of participants, however, had not improved or had worsened at follow-up. Approximately one-quarter of the cohort did not report improvements in pain or disability, and one-fifth were not fully satisfied with the service provided by the clinic.
There was feedback from seven doctors out of 15 who were contacted by mail. Almost all responders agreed or strongly agreed with all seven statements (Appendix 3; available online only), with one disagreeing with the statement ‘the clinic is cost-efficient’. Free-text responses are summarised in Box 1.
| Box 1. Free-text responses from referring doctors |
| What are the most significant issues that continue to affect patients? |
Limited professionals dealing with chronic pain; cost; over reliance on medication; desire for quick fix; follow-up |
| What is working well at this clinic? |
Multidisciplinary care; comprehensive assessment |
| What could be improved? |
Repeated multidisciplinary review; more clinics; more space |
Discussion
Participants with complex persistent spinal pain reported improved function with less pain 2–3 years after a single consultation at this primary care interdisciplinary pain clinic. This study does not delineate the reason for these changes. Around one-half reported clinically significant reductions in pain interfering with activity/mood and overall pain levels. Some participants may be ‘de-medicalising’ their symptoms as they report lower use of analgesics and fewer consultations with health providers while taking more responsibility for their health. Responses from referring doctors suggest they were satisfied with the clinic, and appreciated this type of service being available. Cost and travelling distance seem the main negative elements of the clinic.
An audit of eight private practice clinics that ran chronic low back pain rehabilitation programs based on the Canadian Back Institute model has been published.5 The clinics were run by physiotherapists, occupational therapists, exercise physiologists and psychologists. Patients attended the clinic for one hour minimum, three times per week, over 6–12 weeks. The audit provided data on 899 patients at entry to their program, discharge and six-month follow-up. Average single measurement pain scores decreased by 1.9 on the Visual Analogue Scale, and function improved by 11.3 on a 70-point scale (Canadian Back Institute Questionnaire). This compares similarly to our study.
A prospective study of multidisciplinary tertiary care for chronic low back pain with 12-month follow-up was performed recently in the Netherlands.6 Patients had 16 sessions, each of three-hour duration, over a two-month period, then were encouraged to attend a local health centre twice a week for a further three months. Pain visual analogue scale (VAS) scores dropped from 5.5 at baseline to 3.2 at 12 months, a drop of 2.3. Sixty per cent had a 30% improvement in pain. This compares with 1.7 drop in pain scores and 47% having a 30% improvement in pain in our study.
Both of the above studies involved more intensive interventions than our study; both studies also had less room for individualising management plans. Outcomes were similar.
There has been a recent review looking at the long-term prognosis in persistent low back pain.7 It revealed that patients from a primary care cohort with persistent low back pain do not have widely fluctuating pain. Rather, they tend to have ongoing pain that varies only slightly around their own mean long-term pain. This suggests that for persistent low back pain, improvements in pain and disability are the exception rather than the rule.
There has also been much recent discussion in Australia about the management of persistent pain. Mitchell has called for improved coordination of care in patients with persistent pain.8 He proposed following a model of integrated care between specialists and GPs using case conferences, which has been proven to confer benefits in palliative care and stroke treatment.
Hogg et al2 agreed with Mitchell’s assessment of the disconnect between primary care and specialist pain services. Mitchell thought moves to fix the disconnect were highly likely to improve health outcomes, as did the then CEO of Consumers Health Forum of Australia, Carol Bennett.9 Latimer and Zacest10 commented recently on barriers to spinal pain management in primary care such as limited undergraduate training, lack of consultation time, unrealistic patient expectations of cure and patient demand for the latest investigation or treatment.
A Cochrane review into the multidisciplinary management of low back pain concluded that it was more effective than usual care or physical treatments.
11 The review also noted that multidisciplinary treatment can be costly, time-consuming and resource intensive, putting a considerable financial burden on the patient and the health system.
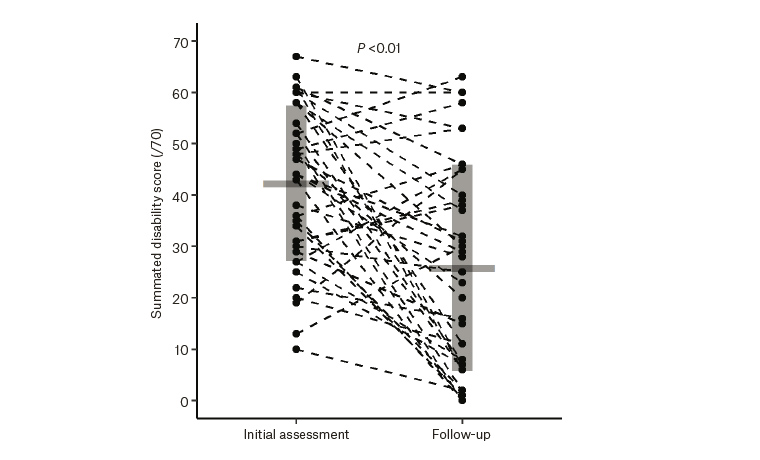
Figure 1. Changes in disability scores
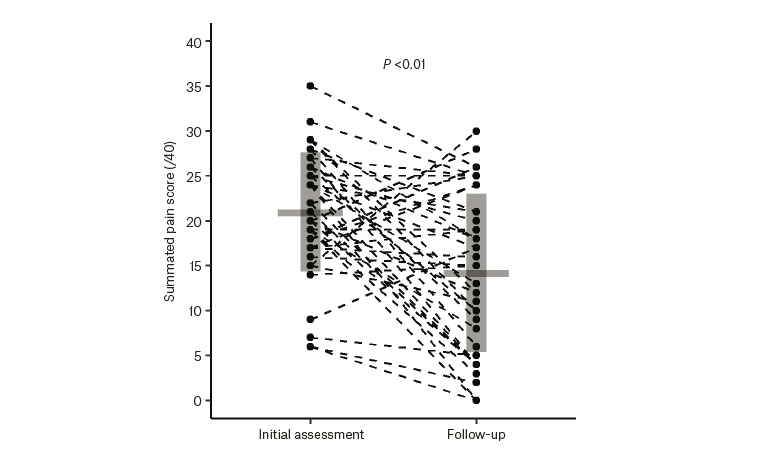
Figure 2. Changes in pain score
Limitations
The limitations of this study include the lack of a control group, heterogeneous pain group, 58% eligible participants and outcomes measured at only two time points. We do not know the full extent of other healthcare that patients accessed after being seen at the clinic. Any improvement or lack of improvement after being seen at the interdisciplinary clinic could be multifactorial and not specifically attributed to the clinic visit. In addition, while independent research assistants conducted the follow-up surveys, the main author (SM) was a practitioner in the clinic, although this clinic no longer operates in the form described.
Conclusion
This audit of a single service shows reports of reductions in pain scores and improvements in activity levels and mood in some participants with complex spinal pain at long-term follow-up of an interdisciplinary pain clinic intervention in a primary care setting.
Ready access to interdisciplinary pain management in primary care may be an attractive option for patients and GPs, and other health practitioners could consider similar innovations tailored to local health needs.
This model of care shows potential for improved management of patients with spinal pain in a timely and economic fashion. Further attention to this model by medical groups, researchers and administrators may be warranted.
Appendices