This article is part one in a three-part series on whole-person care in general practice.
The distinctive value of generalist care has recently received attention in response to increasing population chronic multimorbidity.1–3 The importance of whole-person care (WPC) in this context is recognised.4 WPC (and related concepts of holistic or biopsychosocial care) is a cornerstone of general practice.5,6 However, some suggest that it is not consistently provided.7,8
Previous research conducted by the authors of this article has shown that, in general practice literature, WPC considers multiple dimensions of the person in an integrated way and emphasises the doctor–patient relationship (Figure 1).9 Additional features include recognising patients’ individual personhood, acknowledging doctors’ humanity, viewing health as more than absence of disease, and employing a range of treatment modalities. It was suggested that the term ‘WPC’ more accurately reflects the basis of general practice than the closely related terms ‘biopsychosocial’ and ‘holistic’ care. However, as most included literature comprised theoretical opinion pieces, primary research is required to determine whether the current findings accurately reflect the understanding of WPC among general practitioners (GPs) more broadly. Additionally, these researchers’ previous study did not elicit factors that influence GPs’ provision of WPC.
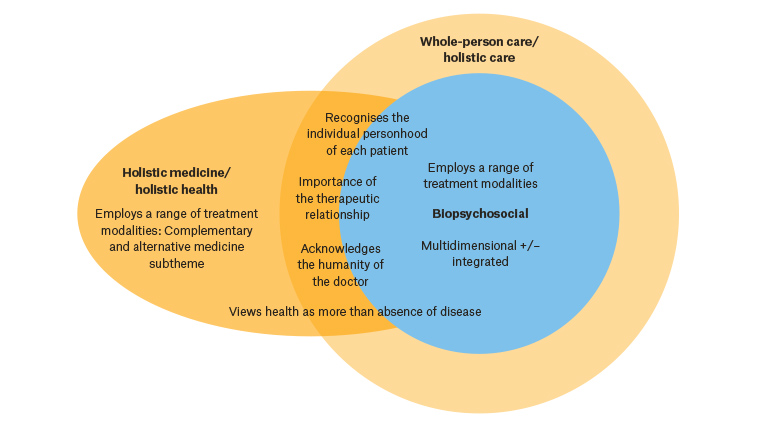
Figure 1. Literature review findings – The elements of whole person care, and its relationship to biopsychosocial and holistic care.9 Themes placed on circles’ boundaries are features of both terms, but more prominent in the term represented by the outer circle.
Reproduced with permission of BMJ Publishing Group Ltd from Thomas H, Mitchell G, Rich J, Best M, Definition of whole person care in general practice in the English language literature: a systematic review, BMJ Open 2018;8(12):e023758.
Therefore, the aim of this qualitative study was to determine how GPs understand WPC and its facilitators and barriers. This is the first of a three-part series reporting the findings of this study. This article reports GPs’ understanding of WPC, the second describes the doctor–patient relationship comprising its foundation, and the third discusses factors influencing its provision. In view of the Australian Government’s current Health Care Homes (HCHs) trial, the researchers also investigated how GPs anticipated that this model would affect WPC.10
Methods
Researcher expertise comprised general practice, palliative care and ethics. Qualitative methodology was chosen to allow exploration of GPs’ views. GPs and general practice registrars practising in Australia were recruited through purposive and snowball sampling to obtain variability in the cohort. Specifically, participants were recruited through Primary Health Network advertising, emailing practices involved in the HCHs trial,11 and using personal, educational and University of Queensland teaching networks. The researchers provided information on the study and obtained informed consent. Participants completed a demographic questionnaire and one 20–45-minute semi-structured interview, conducted by HT. The interview related to the participants’ understanding of WPC, its facilitators and barriers, and how HCHs may affect the provision of WPC. Twenty interviews, 18 by phone, were conducted between May and November 2018, to theoretical saturation. Interviews were recorded and professionally transcribed. Data were analysed using grounded theory methodology.12 Analysis was assisted by NVivo 11 software (QSR International). Two researchers (HT and GM or MB) independently derived initial codes from the data. HT performed subsequent focused and thematic coding, with discussion and consensus achieved between the authors. Additional demographic information was obtained from participants’ practice websites and the Australian Bureau of Statistics’ socioeconomic indices.13
Ethics approval was obtained from The University of Queensland’s Human Research Ethics Committee (2018000558).
Results
Study sample
Nineteen GPs and one general practice registrar were interviewed (Table 1). Participants worked in varied practice settings, with a range of billing structures (bulk, mixed or private billing), governance models (corporate, not-for-profit, doctor-owner), sizes (4–18 GPs according to practice websites, with allied health and visiting specialist services in some practices) and sociodemographic areas. Participants included GPs in both full-time and part-time practice. Seven participants had involvement with HCHs, each with differing attitudes toward the trial. Several participants volunteered during the interview or advertised on their practice website that they were born and/or trained overseas (England, USA, Ireland, Canada and Iran).
| Table 1. Participant characteristics (n = 20) |
| Demographic |
n (%) |
| Sex |
|
| Female |
9 (45) |
| Male |
11 (55) |
| Age (years) |
|
| 30–45 |
7 (35) |
| 45–60 |
9 (45) |
| >60 |
2 (10) |
| Not stated* |
2 (10) |
| Professional memberships |
|
| RACGP |
15 (75) |
| RACGP + ACRRM |
2 (10) |
| No college membership |
1 (5) |
| Not stated* |
2 (10) |
| Time practising medicine (years) |
|
| 5–9 |
3 (15) |
| 10–19 |
4 (20) |
| 20–30 |
5 (25) |
| >30 |
6 (30) |
| Not stated* |
2 (10) |
| Time practising as a general practitioner (years) |
|
| 0–4 |
2 (10) |
| 5–9 |
3 (15) |
| 10–19 |
3 (15) |
| 20–30 |
6 (30) |
| >30 |
4 (20) |
| Not stated* |
2 (10) |
| State |
|
| Queensland |
13 (65) |
| New South Wales |
1 (5) |
| Victoria |
0 (0) |
| Tasmania |
1 (5) |
| Northern Territory |
1 (5) |
| South Australia |
3 (15) |
| Western Australia |
1 (5) |
| Australian Capital Territory |
0 (0) |
| Australian Statistical Geography Standard Remoteness Area34 |
| RA1 |
15 (75) |
| RA2 |
2 (10) |
| RA3 |
3 (15) |
| Index of Relative Socioeconomic Advantage and Disadvantage 2016 (Centile)†13 |
| 2nd–4th |
4 (20) |
| 5th–7th |
6 (30) |
| 8th–10th |
10 (50) |
| Involvement in Health Care Homes pilot |
| Ongoing involvement |
4 (20) |
| Previous or planned withdrawal |
2 (10) |
| Soon to commence |
1 (5) |
| Not involved |
13 (65) |
*Two GPs did not return the demographic information form; their responses are recorded as ‘not stated’.
†Centile 1 represents locations with most disadvantage and least advantage, 10 represents locations with most advantage and least disadvantage
ACRRM, Australian College of Rural and Remote Medicine; GP, general practitioner; RA, remoteness area; RACGP, The Royal Australian College of General Practitioners |
Analysis of results
Prior familiarity with the term WPC varied. Participants nonetheless described similar understandings of the concept. Participants considered that WPC is important and characterises GP care. They described WPC as ‘looking after the patient properly’ (GP02) and ‘what we provide in general practice’ (GP09). However, participants also reflected that WPC is difficult to define, and that ‘because no one’s defined what it is, it’s very hard to know whether they are actually doing that or not’ (GP13).
The analysis identified four themes describing the nature of WPC (Table 2): 1) treats patients as multidimensional persons; 2) length, breadth and depth of scope; 3) based on the foundation of a doctor–patient relationship; 4) may involve team-based care. A model of WPC derived from these themes is illustrated in Figure 2.
| Table 2. The nature of whole-person care – Themes and subthemes |
| Theme |
Subtheme |
| Treats patients as multidimensional persons |
Views patients as persons rather than a series of disease entities |
| Considers the multiple personal and contextual factors that influence patients’ health and treatment |
| Tailors care to the individual person |
| Has length, breadth and depth of scope |
Length: Cradle-to-grave care through repeated consultations over time |
| Breadth: Does not exclude any patient groups or problems |
| Depth: Delves beyond the presenting complaint to address underlying issues and provide opportunistic and preventive care |
| Based on the foundation of a doctor–patient relationship |
Facilitates doctors’ knowledge of the patient |
| Facilitates patients’ trust in the doctor |
| Facilitates management |
| Multifaceted: Encompasses personal, professional and business-transactional dimensions |
| May involve team-based care |
Multiple people provide patient care |
| General practitioner’s role as the ‘conductor of the orchestra’ |
| Team cohesion |
1. Treats patients as multidimensional persons
Participants described WPC as an approach that views the patient ‘as a person, not as a series of disease entities’ (GP12). One GP labelled this ‘the antithesis to disease-based care’, suggesting that ‘there’s doctors who treat patients, and there are doctors who treat diseases’ (GP02). Another described it as ‘treat[ing] them as a whole person, rather than the leg in bed 23, and the eye in bed 1’ (GP09).
Treating the patient as a person involved considering multiple factors that influence health and treatment. Participants implied the importance of scientifically sound treatment, and several stated this more directly when discussing complementary therapy. They emphasised that the scope of WPC extends beyond biomedical concerns to include broader factors such as psychological/emotional health, social determinants of health, family context, culture, spirituality/worldview, environment, stage of life and attitudes toward health. In summary, these included ‘everything that impacts on a person’s life’ (GP10); ‘the whole nine yards’ (GP04). The GP’s role was therefore ‘looking after everything to do with the person or their health at least, as far as we can’ (GP13).
One participant initially expressed a different view, stating they ‘think mostly about the medical conditions … and lifestyle of the patient’ (GP19), and suggested that factors such as spirituality were rarely relevant to care, that discussing them was the role of psychologists and that patients were reticent to discuss them with GPs. However, as the interview progressed, the GP reflected that if patients were willing to discuss these issues this would ‘help me to diagnose better’, and suggested a place for patient education regarding this option.
Providing WPC involved individually tailoring care. One GP stated:
[T]hat’s the whole reason you want to know the patient … each person has a different attitude to care, and what they’re expecting, and what they want from life, and it makes a big difference as to how you would deal with somebody … different people who’ve got superficially similar issues but actually you … deal with them quite differently depending on the person. (GP13)
Several participants believed that this improves outcomes:
[I]f you tailor [care] to the individual, I think you will be more successful. (GP05)
2. Length, depth and breadth of scope
Participants described WPC as having length, breadth and depth of scope.
In terms of length, WPC provides cradle-to-grave care through repeated consultations over time. One GP stated that:
[L]ongitudinally, it’s the care of someone from the … antenatal care when they’re still in utero … through the life span … cradle to grave. (GP12)
Another stated:
WPC goes from the whole spectrum. So, before conception, prenatal counselling … all the way through the years from when babies are first born until people die ... and then even after they’re dead … we’re involved in grief counselling for those who are left behind. So, WPC … is not just from when people are born ‘till they die, but before they’re born ‘till after they die. (GP09)
In terms of breadth, WPC includes all patient groups and problems. One GP described this as:
[Offering] care to all people of all ages and sexes for all of their health needs and problems … issues, concerns, questions … and … try to help with any of those … we would not be saying to anybody, ‘We don’t treat people like you, or your kind of problem’. (GP13)
Breadth of care also involved considering the multiple factors that influence patients’ health, as discussed above: ‘looking after that person’s health and wellbeing … without limiting it to any one area’ (GP12). Participants qualified the GPs’ role in providing breadth of care to that which was ‘within the appropriate limits of our competence and training’ (GP13). Where additional care was required, the GP retained a leadership/coordination role and ‘outsourc[ed] bits of … care as needed’ (GP12).
In terms of depth, WPC delves beyond the presenting complaint to address underlying issues and provide opportunistic and preventive care. One GP identified the importance of exploring ‘the potential underlying issues, not just what’s on the surface’ (GP08). Another felt that treatment may be futile if these underlying issues are not addressed. Using an example of poorly controlled diabetes, they stated:
[W]e can pour as many oral hypoglycaemics into them as we like … but if you don’t understand what … a patient’s life is like … you’re just the Band-Aid. You’re just the ambulance at the bottom of the cliff. (GP15)
Some used government-funded health assessments and care plans as an opportunity to focus on preventive care, while others preferred ‘focused opportunistic approaches’ (GP18) to prevention.
3. Based on a doctor–patient relationship
GPs consistently expressed that the GP–patient relationship is foundational to WPC. Participants’ responses provided insight into the value and nature of the doctor–patient relationship; because of the volume of data obtained, this theme is reported separately in part two of this series.
4. May involve team-based care
Many participants emphasised the importance of involving multiple providers in WPC, and some viewed team-based care as fundamental to its definition: ‘it’s really … teamwork. There’s no way I can do this all by myself’ (GP08). Advantages of this approach included enabling care that GPs did not have time or skills to provide; improving role delineation; increasing patients’ ‘buy in’ (GP17) through reinforcing information; enabling patients to discuss issues and develop relationships with other providers; reducing costs; and improving GPs’ longevity of practice through ‘sharing the load’ (GP09). Some GPs felt that the doctor–patient relationship was enhanced by patients’ relationships with other team members: ‘it might be a [GP] … or a mental health worker … or a mental health nurse … or a … social worker’ (GP01). Others felt that the doctor–patient relationship may be compromised if the GP’s role is reduced to signing off paperwork created by other practice staff, their provision of mental healthcare is decreased, or other providers manage problems that are not referred.
The conceptualisation of team-based care varied between participants, and according to patients’ needs. Team members could comprise practice nurses, other practice staff, allied health, specialists, trainees and patients’ social supports. This varied according to rurality and service availability, and several participants felt that the five annual Medicare Benefits Schedule–funded allied health consultations were insufficient for some patients’ needs. Participants viewed the GP as the team leader and coordinator, ‘outsourcing bits of … care as needed … but … being … together with the patient, the conductor of the orchestra’ (GP12). Several GPs opposed models of care in which other health professionals assumed this role: one reflected that while nurses’ work usually ‘very much complements what the doctors do’, they had stopped employing certain nurses who ‘see themselves as … independent healthcare provider[s]’ and ‘want[ed] to take over the patient care’ (GP20). They described varied models of interaction between team members, from co-located models that enabled shared medical records and informal interaction, to telephone and written communications.
However, some participants reflected that the involvement of multiple healthcare providers did not automatically comprise team-based care. Many identified that the quality of communication between team members varied and was sometimes absent (this topic is discussed further in part three of this series). One questioned the appropriateness of the term ‘team-based care’ to describe health professionals’ interactions:
There are probably groups of … relatively independent professionals who are together trying to look after somebody … so it might be … misleading to call that a team … in the sense of a sporting team, anyway. (GP13)
Another reflected that involvement of multiple providers could reflect competition rather than teamwork:
[A]ll kinds of other people want to get in on the act … so it’s all these competing people … There’s so many people saying they can do parts of the GPs’ job cheaper and/or better … that’s definitely not WPC … that’s actually making it into fragmented care. (GP13)
Discussion
This study found that Australian GPs understand WPC as an approach that treats patients as multidimensional persons; has length, breadth and depth of scope; and is founded on the doctor–patient relationship within the context of a healthcare team. This may result in a general practice model of WPC (Figure 2) that fuses the art of relational, individualised and contextualised care with the science of biomedical treatment.
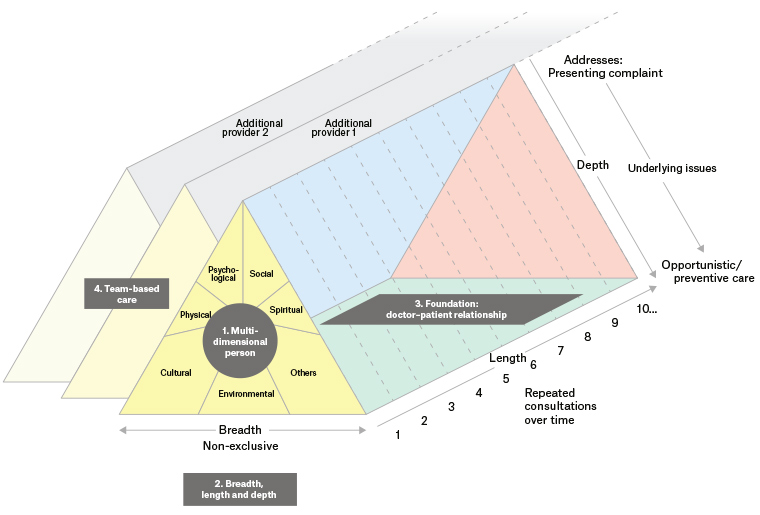
Figure 2. A model of whole-person care (WPC). WPC considers patients as multidimensional persons, has breadth, length and depth of scope, and is founded on a doctor–patient relationship. It may involve team-based care.
The focus on treating patients as individual, multidimensional persons and the importance of the doctor–patient relationship reflect previous literature review findings.9 The current findings further emphasise a team-based approach and the foundational importance of the doctor–patient relationship.
The findings share close similarities with the core values of general practice and the concept of generalism.2,14–16 These emphasise treating the whole person within the context of their illness, continuity of relationship, breadth of knowledge, compassionate care, coordination of care and including subjective factors in medical decision making. Previous research suggests that such values are shared among GPs across broad geographic contexts, from Europe and the Americas to Sub-Saharan Africa.2,5,6,17,18 This suggests that the researchers’ model of WPC encapsulates a foundational construct of general practice care. Additionally, patients relate components of this model, including feeling valued as an individual and the doctor understanding ‘the bigger picture’, to the quality of general practice care.19
Several aspects of these findings deserve further discussion. It was found that GPs believe considering non-biomedical factors is integral to WPC. However, previous research shows differences of opinion regarding the scope of these factors and GPs’ role in addressing them. Spirituality is one example.20 The practice of WPC may vary on this basis.
Second, the findings regarding the longitudinal aspect of WPC correlate with research that shows doctors and patients value relational continuity.19,21,22 Relational continuity encourages trust, enables doctors and patients to know each other as persons, underpins individualised decision making, improves preventive care and reduces investigations, hospitalisations and healthcare costs.21–23 Patients especially value continuity for chronic or sensitive problems.22,24 The findings imply that general practice should facilitate, though not impose, relational continuity to support WPC.
Third, the results indicate that GPs value team-based care as integral to WPC. Team-based care may improve outcomes and job satisfaction.25–27 However, the results are consistent with literature suggesting that involvement of multiple healthcare professionals does not necessarily constitute team-based care: outcomes associated with teams may not be transferrable to ‘groups’ or ‘pseudoteams’, as reflected in some participants’ descriptions.28–30 It is also questionable whether other healthcare providers and patients would agree that the GP (or GP–patient dyad) is the ‘conductor of the orchestra’ (GP12). The resistance of some GPs to others assuming their role suggests issues of power and conflict influencing team dynamics.31 These considerations highlight the importance of carefully considering the nature of providers’ interactions, choosing an appropriate model of interaction, and deliberately facilitating this model. Factors that facilitate team-based WPC are further discussed in part three of this series.
Fourth, it is important to note the similarity of the findings with Aboriginal and Torres Strait Islander views of health. None of the participants currently practised in an Aboriginal community controlled health service (ACCHS), though one who had previously done so spoke favourably of this context. Similar to the suggested model of WPC, Aboriginal and Torres Strait Islander views of health emphasise intergenerational, cultural and environmental aspects in addition to biomedical markers of health.32 This is reflected in ACCHS design and should be explored in future research.
These findings have several implications. The researchers have suggested a model of WPC as understood by Australian GPs, providing a framework that could be used for education, evaluation of the extent to which WPC is currently practised and development of approaches that support WPC.
These results raise additional research questions. The components of WPC exert complex reciprocal influences that deserve further exploration. For example, the interaction between team-based care and the doctor–patient relationship is relevant with proposed shifts from ‘GP–patient’ toward ‘practice–patient’ models of care. Research is also required to evaluate the efficacy of the model; however, outcome measures should be chosen carefully, given the difficulty of quantifying non-biomedical results of WPC.
This study has strengths and limitations. Theoretical saturation was reached, consistent with qualitative methodology, suggesting that this model of WPC validly represents the participants’ views. Limitations include that no participants were currently practising in ACCHSs; this group may provide additional unique insights into the nature of WPC in Australia. While participants otherwise included a reasonably broad demographic of Australian GPs (noting that some demographic data were incomplete or obtained from practice websites),33 it is possible that GPs with an interest in WPC chose to participate, or that participants recruited through similar avenues had shared perspectives, and that the data reflect their views. Future quantitative research could explore whether the findings are representative of Australian GPs’ views more broadly; however, the qualitative results also provide valuable information in their own right. The research focused only on GPs; further studies should investigate other stakeholders’, particularly patients’, views.
Conclusions
Australian GPs understand WPC as a multifaceted approach encompassing many defining characteristics of generalism, encapsulated in the suggested model of WPC. This enables education regarding WPC and provides a basis to assess its current implementation and evaluate its efficacy. The doctor–patient relationship foundational to WPC and factors that affect its provision are described in parts two and three of this series.