Case
A man aged 46 years presented to a multidisciplinary team (plastic surgery, radiation oncology, dermatology) with a year-long history of a lentigo maligna on the right ear lobe. After initial biopsy, the lesion had undergone two wide excisions with his general practitioner (GP). Both excisions showed margin involvement. The GP referred the patient to a radiation oncologist.
The initial referral resulted in onward referral to the multidisciplinary team for assessment.
Examination revealed a well-healed full thickness skin graft with no clinical or dermoscopic evidence of lentigo maligna (Figure 1).
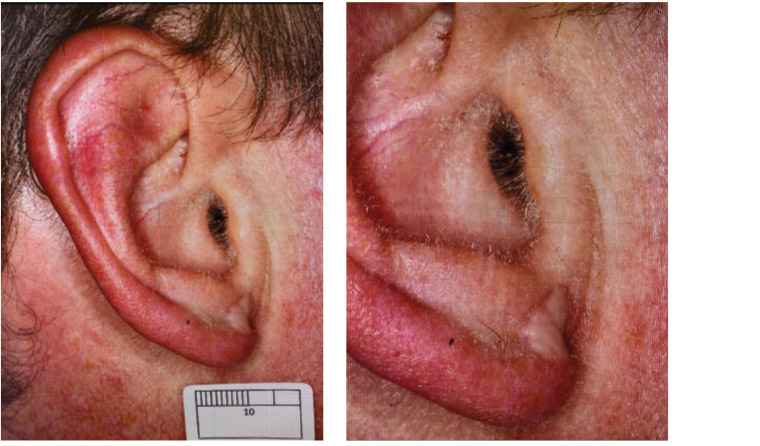
Figure 1. Skin graft scar of right ear lobe
The patient was well, with no melanoma risk factors other than solar damage.
The consensus of the multidisciplinary team was that optimal management would be further excision.
Question 1
What excision margins are advised for lentigo maligna?
Question 2
What are the main concerns with further surgery in this case?
Answer 1
Current Australian guidelines advise excision margins of 5–10 mm around the visible lesion.1 Subclinical extension is more likely with larger lesions and those on the head and neck.1,2
Answer 2
Ill-defined margins and subclinical extension are common with lentigo maligna and, as in this case, lead to involved excision margins.3,4
It can be difficult to differentiate the histopathological appearance of atypical melanocytic hyperplasia seen in sun-damaged skin from lentigo maligna.5 Sun-damaged skin can show features in common with lentigo maligna. This includes melanocytes in higher densities with grouping, follicular extension, cytological atypia and even pagetoid spread into the upper epidermis. This can make the determination of clearance of lentigo maligna difficult.5
A crucial principle is to avoid wound closures that distort the margin until no further excisions are needed.3,6 Complex flaps will distort margins and make re-excision problematic. Reconstruction can be delayed until histopathology confirms adequate clearance.
Confocal microscopy can be used to attempt to delineate the extent of lentigo maligna.7 Another option is mapping biopsies of the surrounding skin to document the presence and extent of residual lentigo maligna.3 Consensus was that these methods would not give certainty to lesion extent.
Case continued
Although there was no visible lesion on which to base margins, it was felt that further wide re-excision would present no significant issues in terms of technical difficulty or functional and cosmetic outcome.
The decision was made to excise a further 9 mm margin around the graft.
Question 3
What non-surgical options are available for management of lentigo maligna?
Question 4
Why was further surgery preferred in this instance?
Answer 3
The main non-surgical options for lentigo maligna are radiation therapy,8,9 topical imiquimod4 and cryotherapy.4
Answer 4
Other options would only be considered when surgery is contraindicated or declined by the patient.6,9 This decision is best made in a multidisciplinary clinic with access to specialist plastic surgical, radiation oncology and dermatological opinion.
Treating lentigo maligna aggressively with surgery is controversial in older people, as it is thought that a small percentage may progress to lentigo maligna melanoma over a long period of time.4 When making a decision not to treat lentigo maligna, the patient’s life expectancy and the fact that the lesion will likely enlarge and may become invasive and thus be more difficult to treat are important considerations. The decision to withhold treatment should be made only after careful explanation to all concerned of the risks involved.4
Radiotherapy carries acute and long-term side effects. In the short term, there is fatigue and skin irritation. Long term, the skin shows poikiloderma with atrophy, telangiectasiae, and increased and decreased pigmentation . Radiation treatment sites are at risk of second malignancy, usually decades later. Thus radiation is avoided in patients aged <60 years where possible.9
Lentigo maligna can be treated definitively with radiotherapy. A large-scale prospective study showed complete clearance rates of 90% for partial surgical excision followed by postoperative radiotherapy, and 97% for wide local excision with complete surgical margins followed by post-operative radiotherapy.4 Radiotherapy alone in a systematic review of 454 patients gave an initial complete response in 87–100%, with recurrences ranging from 0–31%.8
Recurrence rates for surgery are approximately 5%, and this remains the optimal management.10
Cryotherapy for lentigo maligna has been reported in small studies, but evidence is currently lacking to support its use.4 Imiquimod is currently the subject of ongoing trials.4,8
Because for this patient the lesion is now complicated by surgical scarring and is on a high-risk site, neither cryotherapy nor imiquimod is advisable.
Case continued
Unfortunately, the specimen obtained from the third excision also showed margin involvement. A fourth excision achieved histological clearance of at least 5 mm around residual lentigo maligna (Figure 2). The patient remains free of any evidence of local or regional recurrence after 18 months’ follow-up. He has been enrolled in ongoing surveillance and advised on sun protection and the warning signs of skin malignancy.

Figure 2. Final outcome after two further wide excisions and closure with skin graft
Key points
- Optimal management of lentigo maligna is surgical excision.
- As multiple excisions may be needed at times to achieve clearance, closures that can distort margins should be avoided.
- Radiotherapy should be reserved for cases not amenable to surgery. Other therapies lack clinical evidence to support use in lentigo maligna outside of clinical trials.