Case
A man aged 43 years presented with a persistent, progressively enlarging facial lesion that had persisted for more than 20 years (Figure 1). He had a similar lesion on the opposite cheek. He was concerned about the increasing size and associated hair loss of these lesions. The rest of his skin examination was unremarkable, and he was fit and well. He reported that previous biopsy at initial presentation approximately 20 years earlier had confirmed cutaneous lupus, and that his only medication was hydroxychloroquine 400 mg/day, which he had continued since that time. He was also concerned with the long-term risks of hydroxychloroquine and questioned whether other treatments were available.
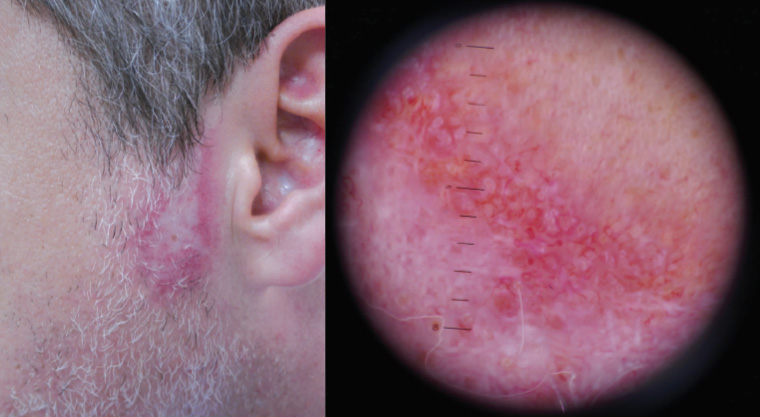
Figure 1. Patient with lesion over pre-auricular area
Question 1
What are the clinical features seen in Figure 1?
Question 2
What diagnoses would you consider?
Question 3
How would you confirm the diagnosis?
Question 4
What further history and examination is needed and why?
Question 5
What would be your further management of this patient?
Answer 1
Figure 1 shows an irregular, depigmented patch within an erythematous halo. Hair loss is evident. Close examination and dermoscopy reveal follicular keratotic plugging, a perifollicular whitish halo and telangiectasias over the pre-auricular area.
Answer 2
This is a longstanding inflammatory lesion that shows both follicular plugging and scarring manifesting as alopecia and depigmentation. The most likely diagnosis is discoid lupus erythematosus (DLE). Lichen planus could produce a similar appearance but would usually be more violaceous in hue.1 Tinea barbae would be unlikely to have such a long history and would typically be more inflamed, or even pustular. The lesion is too inflamed for morphoea, and the follicular plugging would be atypical.1 Given its sun-exposed site, other differential diagnoses include a sclerosing basal cell carcinoma, solar keratosis, intraepidermal carcinoma and squamous cell carcinoma. These would be unlikely, however, given the lesions are bilateral and not of typical appearance.
Answer 3
The first step is to perform a biopsy of the lesion for histopathology.2 One must ensure that actively inflamed skin is captured, rather than the scarred area. Inflamed hair follicles should be included.
Biopsy of the lesion had been performed by this patient’s previous treating clinician prior to this presentation, which was consistent with a diagnosis of DLE.
Answer 4
Systemic lupus erythematosus (SLE) needs to be considered in this patient. The current criteria, as per the European League Against Rheumatism/American College of Rheumatology, for this diagnosis is outlined are Figure 2.3 A thorough history and examination should be carried out for these features.
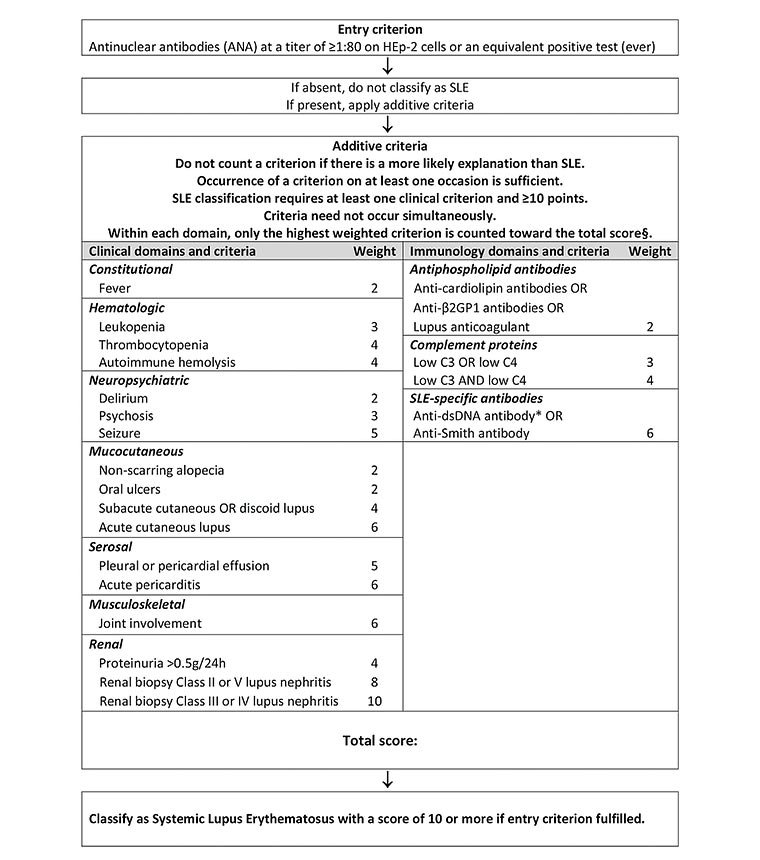
Figure 2. Classification criteria for systemic lupus erythematosus (SLE)
§Additional criteria items within the same domain will not be counted.
*Note: In an assay with at least 90% specificity against relevant disease controls.
Reproduced with permission from Aringer M, Costenbader K, Daikh D, et al, 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus, Ann Rheum Dis 2019;78(9):1151–59, doi: 10.1136/annrheumdis-2018-214819.
Further physical examination should include a full skin examination to look for other lesions, as well as inspection of hair, nails and mucosa. These features were all unremarkable in this patient. Although rare squamous cell carcinoma can complicate lesions of discoid lupus, this should be considered in persistent or treatment-resistant lesions.4
Antinuclear antibody (ANA) positivity is essential to consider a diagnosis of SLE, and thereafter 10 points of additive criteria from multiple clinical domains of the patient are required to confirm SLE.3
This patient was found to have a negative ANA titre. A further history from this patient revealed polyarticular joint discomfort in the absence of any other symptoms, serum or urinary abnormalities. There was no clinically detectable inflammatory joint disease. Additional immunological testing was also unremarkable.
In the absence of any evidence of systemic involvement, a diagnosis of DLE was confirmed. This condition is characterised by scaly annular plaques with a predisposition for the hypopigmentation, scarring and hair loss, as seen in this patient.1,2
Answer 5
The patient should be counselled as to the nature and prognosis of this condition. His risk of developing systemic lupus is low.3,5 Only 18% of DLE cases are reported to progress to SLE within three years of diagnosis.5 The inflammatory component of his condition is amenable to treatment, but the scarring and cicatricial alopecia is permanent.
Preventive measures include strict sun protection, including avoidance, high-potency sunblock and protective clothing. Smoking is a known exacerbant and should be ceased. Topical agents are the preferred option for treatment of localised DLE.2 Potent topical steroids (mometasone, methyl prednisolone aceponate, betamethasone dipropionate) are first-line treatments. They carry risks of skin atrophy and perioral dermatitis, and careful surveillance is needed. As a result of these potential risks, once disease control is achieved, frequency of the topical application should be reduced. If this cannot be reduced to an appropriate level, alternative treatments, including calcineurin inhibitors (eg tacrolimus), intralesional steroid injection or a systemic agent, should be added.2 The minimum effective dose and treatment duration will depend on the activity of localised disease and acute flares.
Systemic therapy is indicated for widespread and/or resistant skin involvement. Hydroxychloroquine is the most commonly used and gold standard systemic agent in cutaneous lupus.2 Systemic therapy is best employed with topical agents. Combined treatment can allow better control at lower doses.2
This patient had been continued on hydroxychloroquine for more than 20 years, and therefore, awareness of the risks and regular monitoring are critical to prevent adverse events. Cumulative toxicity from this agent can lead to permanent retinopathy, cardiomyopathy, serious blood dyscrasias and neurological dysfunction. To prevent this, doses should be kept below 5 mg/kg/day.6,7 Monitoring of full blood count, liver and renal function with baseline ophthalmic examination, followed by annual screening after five years, are needed.8
Case continued
The patient’s hydroxychloroquine was ceased. He was commenced on topical mometasone (corticosteroid) ointment for the two affected sites with significant improvement (Figure 3).

Figure 3. Resolution of lesion after topical corticosteroid therapy
Key points
- Topical corticosteroids are the mainstay of management of cutaneous lupus erythematosus.
- Topical corticosteroids require caution on the face to prevent risk of skin atrophy and other adverse effects.
- Use of topical agents in the treatment of localised disease can allow timely reduction or cessation of systemic agents.