There was a popular meme circulating in 2020 that depicted four older women sitting on a park bench, watching and sharing their observations. The image was captioned ‘For sale: 4 surveillance cameras (old model)’; prescient imagery to frame this article. Whereas ‘old model’ surveillance or observation involves physical presence, contemporary technologies enable observation from a distance that is now part of everyday experiences.1 No longer limited to protecting the public, capturing crimes or, conversely, threatening the loss of civil liberties, the use of video to observe others remotely is now associated with convenience and efficiency.1 Remote video observation provides a ‘mediated visibility’ in which ‘actions and events [are] now severed from the sharing of a common locale and dissociated from the … constraints of face-to-face interaction’,2 enhancing quality control.3
The traditional model of Australian general practice is an apprenticeship model in which trainees are attached to designated general practice supervisors,4,5 gradually increasing the registrar’s work complexity and acquisition of skills.6 Several important activities occur in registrar training: education including workshops, the supervisory support of trainees and the process of observing the consultation through external clinical teaching visits (ECTVs). The ECTV session usually lasts for 3.5 hours and is performed by experienced general practice supervisors or medical educators.7 During the ECTV, the supervisor usually observes the registrar’s clinical consultations with a patient as a silent observer (although there are times at which they may comment), and there is a ‘debrief’ clinical discussion between the observer and the observed between each consultation and/or at the end of each supervision session.
This apprentice-style model has historically relied largely on the registrar and supervisor being co-located in the same room;8 however, it can be difficult to perform in person in rural areas, especially in consideration of ways to enhance training and actively monitor quality patient care.9 In response, video cameras are one type of technology that can be used when the co-location of registrar and supervisor is problematic. Although potentially more impersonal than face-to-face communications,10 unlike other digital media such as email and telephone, video camera use can provide access to non-verbal cues and contextual information to build a greater understanding, which may be missed when using other technology in the consultation setting. Video technology also affords social presence in the application of geographically distanced training.11 Social presence identifies the importance of fostering interpersonal relationships, which are sometimes devoid in distance scenarios.8
Tele-supervision by video has been identified as promoting inclusivity and cost efficiency, a means to overcome space restrictions and travel time, and an opportunity for gaining greater access to qualified supervisors.12,13 There is growing evidence of the effectiveness of remote general practice supervision and consultation observation via technology.14–16 Moreover, with global pandemic disruption, conducting tele-supervision has become the ‘new normal’17 for all, not simply those in rural and remote contexts.
The aims of the pilot study reported on in this article were to investigate attitudes, outcomes and limitations of using live video cameras for distance supervision from the perspective of those directly involved. This investigation not only included the supervisor as observer and the registrar as the observed, but also gained important insights from the eyes of the patients involved.
Methods
Gippsland is located in Victoria, south-eastern Australia, and stretches approximately 41,600 square kilometres, covering 18% of the state.18 A map of the region is depicted in Figure 1.19
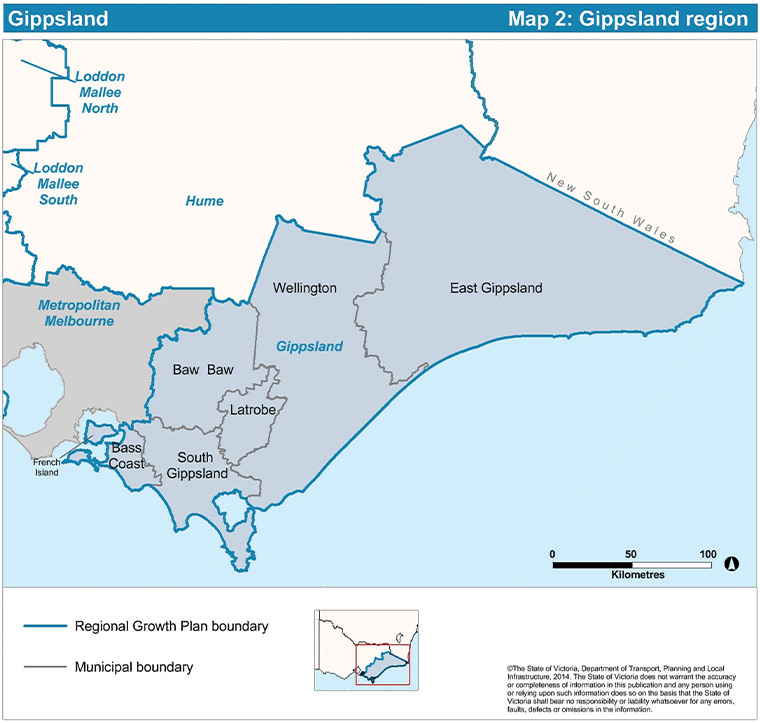
Figure 1. Map of Gippsland, Victoria, Australia19
© State of Victoria (Department of Environment, Land, Water and Planning), licensed under CC BY 4.0 (https://creativecommons.org/licenses/by/4.0)
Gippsland’s population is 271,416,20 many of whom live in small townships or regional centres, with sparse general practice services and training sites.21 For general practice training in this region, registrars’ ECTVs are performed by general practice supervisors.
Commencing and concluding in 2012, a pilot study was undertaken in Gippsland using video cameras to facilitate remote supervision of registrars. The pilot involved installing a video camera network at participating general practices using real-time video only, with the recording functionality disabled. The supervisor and registrar were not co-located; however, registrars had access to a clinical supervisor on call in the clinic should they be required. The consultations themselves were not the focus of the research; rather, the aim was to explore the effectiveness of off-site supervision via real-time video through the experience of the participants (supervisors, registrars and patients). Details of the video camera technology used in the pilot study are outlined elsewhere.22
A constructionist theoretical paradigm was followed, which indicates that all knowledge and meaning is socially constructed and contextual. This epistemology posits no single ‘truth’ but takes into account multiple perspectives,23 a pertinent approach for the researchers, who wanted to hear all participants’ views with equal weighting.
In line with research ethics approval (Monash University Human Research Ethics Committee ethics number CF11/2621 – 2011001533), general practice supervisors in Gippsland were invited via a research flyer distributed to general practice clinics through Southern GP Training to be involved in the video camera trial with their registrars. The names and contact details of those supervisors responding to the call were then passed on to researchers at Monash Rural Health to organise the pilot evaluation interviews. Written consent of participating supervisors and registrars was taken at the beginning of the project.
Patients were first notified of live video sessions when making an appointment booking with the registrar and again at reception on arrival. Consent was also sought before commencing the live video session; the registrar explained the security and privacy measures to the patient using a written protocol. This information gave the patient several opportunities to confirm their voluntary participation in not only the video camera pilot, but also the subsequent interview.
Four supervisors and seven registrars from six general practice clinics in Gippsland took place in the pilot. Along with 18 patients, the participating supervisors and registrars were interviewed by independent interviewers from Monash Rural Health to identify enablers and barriers to using real-time video for supervision. The interviews were semi-structured, focusing on the 1) experience of the technology and 2) impact of the technology on the educational experience. All interviews were conducted face to face in a separate room in the participating surgery. Guidelines for the semi-structured interview questions were used for consistency (Appendix 1); the first for the supervisors and registrars and the second for the patients. The supervisor and registrar’s individual interviews lasted up to one hour in duration. For the patients, the interviews were brief and up to 10 minutes in duration, taking place immediately following their clinical consultation, with the registrar confirming the clinical capacity of the patient to engage in the interview.
Interviews were audio recorded, transcribed and anonymised to protect privacy. Participants were ascribed an identifier commencing with ‘S’ (supervisor), ‘R’ (registrar) or ‘P’ (patient) and then numbered. The interview transcripts were jointly analysed thematically24 using a constant comparison technique17 to investigate attitudes, outcomes and limitations of the video camera technology. With this careful and rigorous activity of refining, defining and discussing, the data were coded to key emergent themes through an iterative workshop process whereby multiple analysts investigated each part of the data to come to a consensus. This technique allowed the exploration and comparison of participants’ comments.
While original analysis of interviews was completed in 2013, in light of the global COVID-19 pandemic, the data were revisited in 2021 by two of the original researchers (MS and JB) alongside a new researcher (JW). Further literature, knowledge and insights gained since 2013 thus reflect and build on the original research.
Results
Following the process of constant comparison to analyse the interview transcripts, key themes emerged from the data, from positive to negative. To amplify each of these themes, participant quotes are excerpted and discussed, edited for clarity where necessary.
Positive perspectives
Positive research themes included: flexibility, closing the geographical gap, reducing travel time, being less intrusive than an in-clinic observer, modernising, enhancing the training experience and increasing expertise in the consultation.
One of the main advantages of video technology is its flexibility, providing supervisors with the opportunity to fulfil their regular responsibilities in clinics without the need for supervisors and registrars to be co-located. The technology enabled supervision to extend beyond ‘one room in one clinic relating to one registrar in one clinic’ [S2]. This flexibility also increased communication possibilities and the ability of registrars to contact their supervisors, providing the ‘ability to become much more flexible with the training and the ability to keep doing my role’ [S4]. This benefit was also articulated as closing geographical gaps:
I was quite excited that it … was possible to be able to get this infrastructure in so that we can actually start to supervise registrars remotely … I can see real benefits, but if the technology’s honed and we know how to use it well ... [then] we can start to bridge some of the geographical gaps. [S1]
The technology also enabled multi-site interoperability:
We’ve got [other] branches … so we’ve actually got different sites that we work in, and it gives me a greater option for supervision. [S2]
An important benefit of video cameras, as noted by most of the supervisors, was that time and travel costs were substantially reduced. As one supervisor noted:
I think the biggest benefit is ... not having ... to drive and … if we’ve got, say, an afternoon session, [not to] spend two hours driving. [S2]
This was also echoed by a patient, who stated that video supervision ‘decrease[s] the [travel], and the cost and … increase[s] the effectiveness of it, so … of course it’s an advantage’ [P11].
For registrars, there was the perception that video camera use for supervision was advantageous in their training:
I think that it … is a good tool … it’s not changing how the registrars are getting their education, and it’s just a different mode of doing the same thing. [R6]
For supervisors, the potential benefits in the educational process of registrars of tele-supervision via video cameras related to overcoming barriers and increasing their access to specialists, with one commenting that a key benefit is ‘particularly with specialists visits [as we] start to utilise that technology more’ [S1]. One supervisor noted it:
Also hopefully gives a better training experience to the registrars because they can get hold of me easier. We can go face to face, you know, whereas before we had to mostly [talk] over the telephone. [S4]
With the impact of COVID-19 and contemporary rise of telehealth, these comments are pertinent. Patients also highlighted the benefits of video technology, especially in rural areas:
I can see it [might be] very beneficial if there was something serious happening and you wanted a doctor, especially in a country area, wanted to have a second opinion … I think it’s fantastic technology really and anyone who says ‘oh I’m self-conscious of that thing up there looking at me’ well, I think they need to see another doctor because the fact is it is really a very effective system of operating … [T]his sort of thing is really good and in teaching, fantastic for teaching. [P1]
One patient noted that the video technology is useful for having a confirming viewpoint in the consultation:
I suppose it’s always a second opinion they could fall back on, if required … [It’s] the way of going forward I suppose. [P9]
Another commented on tele-supervision increasing expertise in the consultation, a bonus ‘second opinion’:
If I was having an examination for something serious and there’s another doctor watching, it’s quite beneficial because if they talk to one another, it’s really like a double go, isn’t it? In fact, if I was having something serious, I wouldn’t mind another doctor being present, and that’s really what will happen. You know I could see that if I had something bad with me, another specialist sitting on that screen up there looking at me, I would feel very comforted by that. [P1]
Some supervisors suggested that conducting supervision via the video camera could be less intrusive than traditional co-located supervision, potentially lessening the anxiety of the registrar being observed:
One of the issues about ECTV is … having somebody else sitting in the [room] … can make the registrar who’s being visited a little bit more anxious and aware when there’s somebody sitting there ... it might lessen that anxiety a little bit if it’s done via camera. [S3]
From the patient perspective, the impact of technology on the consultation was apparently not an issue. While one patient stated that it was in the back of their mind that they were being observed, they also noted: ‘I was crook, so it didn’t really worry me’ [P2]. Another patient spoke about finding the technology non-intrusive: ‘You just ignore it and I’m there to see a doctor, not [the supervisor], so … it was all good’ [P5]. Some patients commented that they even forgot the camera was on: ‘I just forgot [the supervisor] was there’ [P7]. Similarly, ‘I didn’t really notice them so … it’s not … something that’s like … “camera, action”’ [P8]. Another had forgotten once the consultation was underway that the camera was on, only becoming aware when the supervisor made a comment: ‘until [they] spoke up … you’re like, “oh yeah I forgot”’ [P6]. A further patient expressed comfort with the use of video camera technology during their consultation:
It didn’t worry me at all … [It was a] conversational thing about my health … it really was at a level which was quite discussable… I didn’t even think about it … it was unobtrusive, it wasn’t sitting in your face. I was shown it. Time was taken to show it to me. So, it was really of no great consequence to me. I really didn’t care. [P1]
Another patient also highlighted the importance of the positioning of the technology in the consultation space as the camera had been placed somewhat discretely by the doctor:
I think [the doctor] did a good job, because [they] had it strategically placed where it was … I virtually couldn’t see the screen, it was facing [the doctor] and the camera was coming out, so that took your mind off it all quite a bit. [P2]
One patient expressed surprise, being somewhat in awe that such contemporary video technology would be available in an often under-resourced rural area:
I was only surprised that it is up here, like in the country because you don’t get much technology up here, do you? You can’t get a doctor up here! [P2]
In conclusion, the positive perspectives highlighted by the research participants indicate the potential of video cameras for remote supervision, which are applicable not only for regional, rural and remote locales, but also during times of crises.
Negative perspectives
Providing a balanced perspective, this section explores some of the challenges experienced with technology for remote supervision. Negative themes included: confidentiality issues, lack of personal engagement, the loss of serendipitous ‘corridor conversations’, professional development in use and technical issues relating to connectivity.
The potential of intrusiveness of video was also raised by some participants as a negative. One patient stated that the video camera ‘did kind of intrude on the conversation a little’ [P11]. Another added: ‘Yeah, I was aware of it because I could see the other [doctor] on the screen’ [P4]. This is a consideration in the initial setup and placement of both the video camera and screen.
Concomitantly, some patients noticed an element of artificiality with the video process, which felt somewhat contrived:
A couple of times I was looking at myself … thinking ‘am I trying to make [the doctor] feel good about themselves?’; my body language was leaning way towards [the doctor] … I was sitting rather awkwardly. I generally sit back and discuss … See now that was rather strange for me, now why I did, I don’t bloody well know! [P1]
Ironically, while noted as a benefit for some, the video camera was seen as a potential barrier by others: ‘at first it’s different or weird but then it was alright’ [P6]. Clear explanations to the patient are warranted if the video camera is being used for tele-supervision purposes. It is vital that doctors ensure that patients are comfortable with this type of technology and are fully informed before its implementation. As one patient noted, it can be a little awkward: ‘I’m just not used to it that’s all’ [P4].
One supervisor was concerned that using videos for conducting consultation observation visits would replace the opportunity to engage with other doctors and registrars in practices being visited. There was a genuine fear that this unique dimension of the consultation observation visits might be lost if the video camera replaced face-to-face visits:
To get out and smell the roses, go to another practice, see how they do things, just get a general impression … you take back a different impression about how you might do something … I’ve really enjoyed going to the different centres, meeting the different staff, the doctors, and of course sitting in with the registrars and just really seeing how they do it. [S4]
While a useful tool, some noted that technology does not replace face-to-face communication. For example, one registrar noted:
It’s just a different mode of doing the same thing perhaps saving time … in terms of travel … bearing in mind that it has its own limitations. It doesn’t replace … the face-to-face experience. [R6]
One of the supervisors highlighted the importance of personal interaction in a registrar’s training, commenting that it is ‘always nice to shake someone’s hand and to encourage them to watch what’s going on’ [S2]. This quote highlights the affective nature of such face-to-face interchanges and how they affect other aspects of supervision, such as a feeling of belonging and engagement, that cannot necessarily be replicated by remote supervision.
Supervisors were concerned that distance supervision using video cameras would reduce the amount of personal contact, interactions and flexible spontaneous ‘corridor conversations’ that they would be able to have with registrars in the face-to-face context. Corridor conversations – or clinical communication in open spaces25 – are an example of ‘serendipitous learning’, defined by Bowles26 as knowledge that ‘happens by chance, or as a by-product of the main task’. Corridor conversations involve situated learning and relate to the immediacy of the ‘now’. These informal conversations provide a variety of uses in the training context and can be classified into five different purposes: clinical, technological, organisational, affective and reflective.25 Further, corridor conversations can contribute to patient safety27 by providing registrars immediate feedback on concerns that are time-sensitive matters that might be forgotten at the end of a long day, or pastoral issues noted by the supervisor in relation to the registrars. One supervisor raised concerns about the potential loss of accidental contact that occurs on site, suggesting that ‘we’ve got to build capacity in for some of that … sort of pastoral stuff to happen’ [S3].
Supervisors noted that throughout the educational process of registrar training, good quality supervision was a top priority, regardless of the medium used:
[W]e are going to have to think of ways of making sure, even though this is happening; making sure that there is good supervision happening as well. That’s the main purpose of being here and for us doing it. [S2]
The notion of the value of quality supervision was reinforced by the registrars:
[I]n the traditional setting … the supervisor comes around and sits with us. [It] doesn’t replace the … face-to-face experience. In fact, there is a risk of losing some aspects of the … original process but if circumstances are limited this is your alternative. [R6]
In addition to having confidence in the technology, some supervisors raised the issue of confidence in terms of patient confidentiality – indeed, that this might be the ‘biggest issue’ [S2]. One of the supervisors noted that if someone came into the room of the viewing supervisors, there could be a serious breach of patient confidentiality, a point captured by a patient:
At one stage [the registrar] thought that [they’d] lost [the supervisor] but actually hadn’t. [The supervisor] said ‘Oh, no, I’m fine. I’m still here.’ I don’t know what happened, but someone came into the room at [the supervisor’s] end but there was no problem. [P10]
Another issue raised by participants was the need for training of doctors in the use of video technology for tele-supervision. S4, for example, emphasised the need for clarity and simplicity and claimed to be a ‘dinosaur’ with technology, making an argument for the ‘Keep It Simple, Stupid’ approach.
The final issue raised by participants was potential technology-related problems, including internet connections and connectivity, server issues and about knowing ‘what to do if the software falls off’ [S2]. Participants stressed that the video technology needed to work well and should not be ‘too clunky and difficult and pain in the arse!’ [S3].
Discussion
The delivery of supervision and consultation observation via live video cameras has distinct merits and limitations that must be understood for its adoption in clinical supervisory settings. Overlaying both the opportunities and challenges discerned in this study was the underlying caveat that no matter what the modality of supervision (face-to-face or electronic), the facilitation of quality supervision is paramount.
Positive aspects of video technology included flexibility, provision of supervision for non-co-located registrars, lack of intrusiveness if the video and screen are set up correctly, and the reduction in travel time. Negative themes included the need for training in the technology, potential disruption with internet connectivity and stability, and the possible loss of learning that takes place in serendipitous corridor conversations.28 Moreover, a key issue raised by participants concerns patient confidentiality. Related to this is ensuring observers are on ‘mute’ and that the session they are observing cannot be overheard by others at their end. The wearing of headsets or earphones can overcome this challenge.
The findings of this research not only capture the rich participant voice of experience, but also add evidentiary support to other position papers on the topic of remote supervision,17 emerging research on the provision of remote supervision29 and the development of remote supervision guidelines from general practitioner colleges30 and other training organisations. The findings also support successes and concerns that are being heard anecdotally from those in the field of general practice training, pointing to the need for sector considerations.
There are several important implications for future research that can be drawn from this study. The first is that timely and comprehensive evaluation strategies must be adopted to investigate the integration of video technology for live non-co-located supervision. Second, perspectives of patients as stakeholders should be incorporated into studies that explore video use for tele-supervision. Further, as videos have been used successfully in other supervisory contexts that involve distance learning,8 the technology could be used for peer teaching and learning, international learning opportunities and supervising medical students. The main limitation in this project was that it was constrained to a pilot study in Gippsland; it did not include experiences of those in urban settings, those in other states or those using the technology offshore. Future research might also consider gauging from participants their considered balance between the positives and negatives in the use of the technology.
Conclusion
Remote supervision is no longer the realm of those geographically distanced from one another. The global pandemic has levelled the supervision ‘playing field’. While the technology and clinical, public health and social environment have changed rapidly since the pilot and interview data collection took place, the experiences of users remain relevant in tele-supervision via video. This research highlights several implications for practice, providing an evidentiary base for remote supervision via video, from positives to challenges. Moreover, the findings reflect that the benefits of video implementation outweigh the negatives and that these can be overcome by application of and adherence to current national guidelines and preparation.30 Many examples of video tele-supervision in the literature involve only a supervisor and the trainee;13 this research adds insights from the patients’ experience as well. While acknowledging that research is currently being conducted in video supervision and remote supervisory models, we recommend that further research continues to be conducted in this space.