This article is part two in a three-part series on whole-person care in general practice.
Whole-person care (WPC) is foundational to general practice, and relevant as chronic multimorbidity increases internationally.1,2 However, it may not be consistently practised.3 A previous systematic review conducted by the authors of the current study identified the features of WPC in general practice literature.4 Whether these reflect the views of Australian general practitioners (GPs) and the factors that affect their provision of WPC remained unclear.
This qualitative study was conducted to determine Australian GPs’ understanding of WPC and factors that affect its provision. A resulting model of WPC was suggested in part one of this series (Figure 1).5 The foundation of this model comprises the doctor–patient relationship. Because of the richness of the data related to this theme, this article reports it separately.
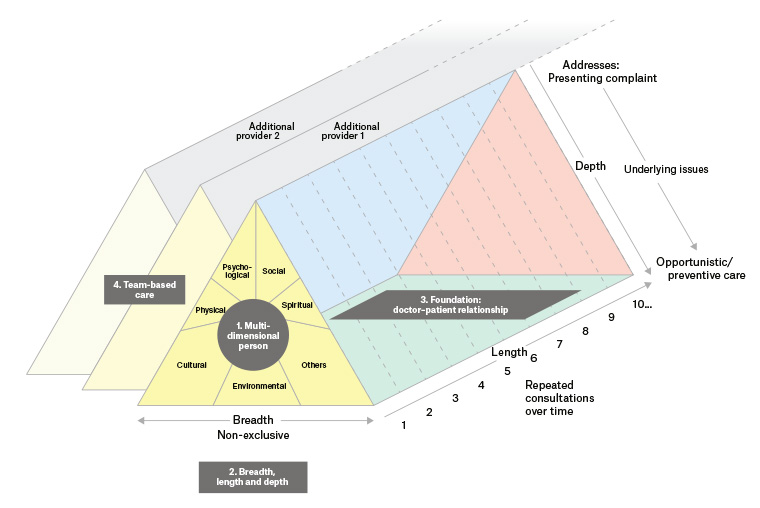
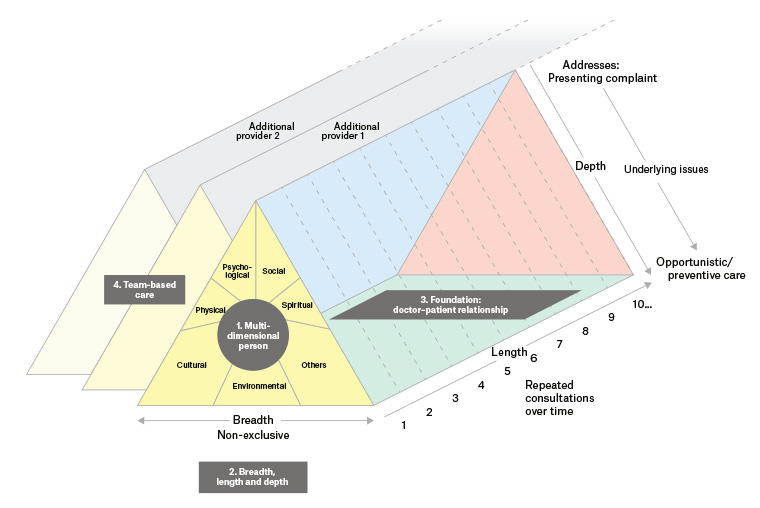
Figure 1. A model of whole–person care (WPC). The doctor–patient relationship is foundational to WPC. It facilitates knowing patients as multidimensional persons, and trust that enables length, breadth and depth of care.
Reproduced with permission of The Royal Australian College of General Practitioners from Thomas H, Best M, Mitchell G, Whole-person care in general practice: The nature of whole-person care, Aust J Gen Pract 2020;49(1–2):54–60, doi: 10.31128/AJGP-05-19-49501.
Methods
Study methods and participant characteristics are reported in full in part one of the series.5 To summarise, GPs or general practice registrars practising in Australia were recruited and participated in a semi-structured interview concerning their understanding of WPC and its facilitators and barriers, and how they anticipated the introduction of Health Care Homes would affect the provision of WPC.6 Interviews were transcribed and analysed using grounded theory methodology.7
Results
Nineteen GPs and one general practice registrar were interviewed. Participant demographics are reported in part one of the series.5
Four themes were identified describing the nature of WPC (Table 1; Figure 1). The third theme, the doctor–patient relationship as foundational to WPC, is the subject of this paper; its subthemes are listed in Table 1. Participants emphasised its importance. One stated:
[A]t the end of the day … whole-patient care … is about the will and the … skill of the doctor to develop the therapeutic relationship with the patient. (GP02)
Others described it as ‘critical’ (GP15); ‘pivotal, central and crucial’ (GP06); ‘the gem of medical care’ (GP02). One GP suggested that this relationship may develop with other members of the practice team:
[I]t might be a [GP] … or a mental health worker … or a mental health nurse … or a … social worker. (GP01)
| Table 1. The nature of whole-person care – Themes and subthemes |
| Theme |
Subtheme |
| Treats patients as multidimensional persons |
Views patients as persons rather than a series of disease entities |
| Considers the multiple personal and contextual factors that influence patients’ health and treatment |
| Tailors care to the individual person |
| Has length, breadth and depth of scope |
Length: Cradle-to-grave care through repeated consultations over time |
| Breadth: Does not exclude any patient groups or problems |
| Depth: Delves beyond the presenting complaint to address underlying issues and provide opportunistic and preventive care |
| Based on the foundation of a doctor–patient relationship |
Facilitates doctors’ knowledge of the patient |
| Facilitates patients’ trust in the doctor |
| Facilitates management |
| Multifaceted: Encompasses personal, professional and business-transactional dimensions |
| May involve team-based care |
Multiple people provide patient care |
| General practitioner’s role as the ‘conductor of the orchestra’ |
| Team cohesion |
| Reproduced with permission of The Royal Australian College of General Practitioners from Thomas H, Best M, Mitchell G, Whole-person care in general practice: The nature of whole-person care, Aust J Gen Pract 2020;49(1–2):54–60, doi: 10.31128/AJGP-05-19-49501. |
The effect of the doctor–patient relationship
Facilitates doctors’ knowledge of the patient
Participants indicated that the doctor–patient relationship enabled them to know the patient as a person. This facilitated understanding the factors contributing to patients’ health issues, treating them as multidimensional people and providing advice tailored to context: key features of WPC. One GP described WPC as having ‘someone who knows us [patients], understands us and can work with us on maintaining our health …’ (GP12). Another reflected:
[T]hat’s definitely not something you can follow a guideline for. You have to know the patient for … a period of time … look after some of their other illnesses and know how they deal with that … know in general what sort of person they are … how effective … care can be [comes down to] knowing that ground. (GP01)
Facilitates the patients’ trust in the doctor
Additionally, GPs identified that building a doctor–patient relationship facilitates patients’ trust in the doctor. This supported WPC in several ways. Patients were more likely to disclose information, particularly regarding psychosocial concerns, after establishing trust:
People don’t just sometimes know if they’ve got permission even to, to waste the doctor’s time with certain things, so they … come in with something and then discover if they can talk to you … they’ll open up on, [disclosing] stuff … that might be upsetting them, making life difficult for them. (GP18)
[P]eople felt after a while that they could share with you sometimes things that they’d never shared with people before … and that was a real privilege. (GP16)
This disclosure facilitates the depth and breadth characterising WPC. GPs also believed that patients were more likely to return when there was a trusting relationship, facilitating the longitudinal aspect of WPC.
Facilitates management
Participants believed that the doctor–patient relationship facilitates management. It allowed shared decision making and facilitated adherence to management recommendations:
[T]his trust in this relationship is the cornerstone … if they trust … me they will following everything … or at least most of it. (GP19)
Conversely:
[I]f the patient doesn’t believe you, it doesn’t matter what you say. (GP17)
Additionally, one GP expressed that a trusting relationship created a context in which, over time, they were able to sensitively question and challenge behaviours, fears and worldviews that they believed were detrimental to patients’ wellbeing.
The nature of the doctor–patient relationship
Participants’ descriptions of the doctor–patient relationship encompassed professional, personal and business-transactional dimensions.
Professional dimensions
An element of professional duty undergirded the doctor–patient relationship. One GP described caring about the patient as professional duty:
[A]t the end of the day … trying to get the doctor to care about the patient is a medical profession[al]’s duty to … be professional … (GP02)
Another described a responsibility to ‘bury [their] own feelings’ (GP03) toward patients with whom they had difficulty connecting for personal or moral reasons, in order to develop a doctor–patient relationship that facilitated care. However, this duty was not necessarily absolute. One GP expressed:
[T]here are always going to be some people where you just don’t gel with them … and I think … we all come to a realisation sooner or later that there are some people that we are not, perhaps the best doctor for, and that’s okay as long as there’s someone else out there who can fulfil that role. (GP12)
Personal dimensions
Personal elements also characterised descriptions of the doctor–patient relationship. Some GPs described providing encouragement, affirmation and unconditional acceptance toward their patients. With long-term continuity, some GPs reflected that these relationships could resemble friendships: ‘Some patients are very comfortable … they’re just like friends’ (GP19). Another GP described ‘loving’ their patients:
[A]cknowledging them as people … warts and all … caring about them more than just their illness … being interested in their life … maybe opening up … ‘What are your thoughts about death and dying … illness … have you got a spiritual basis?’ ... their worldview influences. (GP16)
This GP’s description of farewelling a practice captured the depth of the personal aspects that may be present:
[T]he last time [the patients were] giving me hugs and … crying. And [I was] saying, ‘You know what, we walked a really long journey together … haven’t we … we’ve helped to grow … and we’ve been there for each other and ... I diagnosed your cancer and you got through that. And then you had the other thing and I’m so proud of you … I’m so impressed … at … the way you’ve walked your journey’. (GP16)
However, this type of doctor–patient relationship was not universal: the GP who reflected that some patients are ‘just like friends’ noted that others ‘are very resistant and guarded’ (GP19). This distinction was largely dependent on interpersonal factors, discussed further in part three of this series.
An additional aspect of the personal dimension of the doctor–patient relationship was an element of mutuality. Participants identified that the patient knows the doctor, at least to some degree. For this reason, the person and behaviour of the doctor were relevant to care. Some GPs described circumstances in which patients noticed doctors’ personal health behaviours. Others described occasionally, in carefully selected circumstances, disclosing personal experiences to their patients with therapeutic intent (eg to develop rapport, express empathy or reduce patients’ sense of stigma). Despite this, GPs commented that requiring doctors to act as role models was ‘dangerous territory … you can’t have every doctor being svelte and fit’ (GP07). They emphasised that doctors’ professional competence should be judged by their patient management rather than by their personal health behaviours. Several suggested that imperfection could even be beneficial:
[T]he patients like to relate to doctors as well. (GP07)
[I]t’s important that we are seen as human … and that we are not perfect … I like to be human and create a bit of … relationship. (GP05)
[I]f you are not perfect and you can convey that to your patients who aren’t perfect, then you are probably better at encouraging them to just have a go. (GP07)
Business-transactional dimensions
Participants also described business-transactional dimensions in the GP–patient relationship. Participants worked in bulk-billing, private-billing or mixed-billing practices. Some suggested that private billing could increase the personal investment of both doctors and patients in the consultation:
The doctor has to … justify that money so he has a nice healthy therapeutic … relationship. (GP02)
[I]f people don’t pay for [care] … they don’t value it. (GP10)
Conversely, some participants identified that private billing could disrupt continuity of care where multiple visits were required and could not be afforded, or where patients suspected that doctors were trying to maximise billings through repeated visits. Participants also viewed the business dimension as a barrier to WPC if doctors’ primary focus was on maximising profit, and some implied that this sometimes occurred with colleagues. However, several expressed a personal willingness to provide WPC at financial cost to themselves. One stated:
[Practising WPC] often came at a cost financially to me because I wouldn’t make as much money, but it was easy in the sense that I could … practise in the way … I felt it was appropriate to practise medicine. (GP16)
GPs described interactions between these professional, personal and business-transactional dimensions, which could enhance or detract from the quality of the GP–patient relationship.
Discussion
The doctor–patient relationship was foundational to GPs’ descriptions of WPC in this study. Participants expressed that a healthy doctor–patient relationship enabled the doctor to know the patient and supported patients’ trust in the doctor. This supported the multidimensional, personally tailored and broad scope of WPC. It also facilitated management through shared decision making, encouraging compliance and creating a context in which the GP could sensitively challenge factors they believed were detrimental to patients’ health.
Participants’ responses implied that the doctor–patient relationship was unique and multifaceted in nature, encompassing professional, personal and business-transactional dimensions. These were interwoven, exerting complex reciprocal influences. For example, the personal dimension of the doctor–patient relationship was sometimes described like a friendship, but also occurred in a professional context in which the doctor’s duty of care sometimes required ‘bury[ing] … [their] own feelings’ (GP03) towards patients for whom they did not have a natural affinity. Similarly, the personal dimension of the relationship could facilitate trust, while its business-transactional dimension could challenge trust if patients believed doctors were trying to maximise their billings.
The results are consistent with previous patient perspectives that relate ‘holistic care’ to ‘“good” patient–doctor relationships’.8 They provide evidence that GPs, like patients, view the doctor–patient relationship as fundamental to WPC. They also share striking similarities to previous descriptions of the doctor–patient relationship. On the basis of a systematic review of patients’ perspectives, Ridd identified trust, knowledge and regard (likened to friendship) as three of the four elements that comprised depth of the relationship; the fourth element in their model was loyalty.8 Similarly, in separate studies conducted in diverse cultural contexts (USA and Iran respectively), both Scott and Razzaghi identified trust and a ‘sense of being known’/‘being acknowledged’ as two of the three relational elements of healing relationships; both identified hope as the third element.9,10 Additionally, previous research supports participants’ perceptions that a healthy doctor–patient relationship facilitates patient disclosure of sensitive information and compliance.11–13 Research also suggests that this relationship increases patient satisfaction and may improve clinical outcomes.14–16
The importance of personal aspects of the doctor–patient relationship featured prominently in these results. Some participants’ comparisons of the relationship to friendship and one participant’s reference to ‘loving’ patients reflect previous research. Other studies have drawn comparisons with family relationships.8–10 The accuracy of these comparisons is debated: while acknowledging that the doctor–patient relationship is personal, some have highlighted its differences from other friendships, and the potential for boundary violations.17,18 The asymmetry of the doctor–patient relationship due to its inherent power differential and patients’ vulnerability is perhaps the primary factor differentiating it from other friendships.18 Nonetheless, personal factors including valuing the person without judgement, commitment over time and managing power in a way that is beneficial to the patient have been found to characterise healing relationships.9,10 The importance of love (‘agape’) as deep altruistic care has also been discussed in literature from other health disciplines.19,20 Clearly, a ‘one size fits all’ approach to the doctor–patient relationship is inappropriate. Contextual factors are important: for example, differences in the nature of GP–patient relationships have been observed in rural versus urban communities,21 and the rural context may pose specific challenges related to personal–professional boundaries. However, the personal aspect of the ‘art’ of medicine should be acknowledged and further explored, and its appropriate expressions supported.
One aspect of the personal dimension of doctor–patient relationships that engenders particular debate is the appropriateness of doctors’ self-disclosure to patients.18,22–27 This has traditionally been discouraged because of the perception that the doctor should be a detached observer, and concerns regarding boundary violations.18,23 Nonetheless, previous research suggests that brief self-disclosures to patients occur relatively frequently.22 These may be irrelevant to patient needs, and carry risks.18,23,27 These include risks to the doctor (eg related to privacy, reputation, professional boundaries), which may be amplified in a small-community context. However, self-disclosure may also have beneficial effects within specific parameters: most notably, when serving patients’ (rather than doctors’) needs.23–27 Self-disclosure has therefore been accurately described as a ‘high risk, high gain investment strategy’.23 While previous research has begun to elucidate the nature and circumstances of helpful self-disclosures, further work would help to clarify its role.
Previous literature has proposed a variety of models to describe the doctor–patient relationship and debated whether these accurately describe its nature.9,28–31 The authors of the current study do not present a fully developed model of the doctor–patient relationship, but these findings suggest that it comprises multiple interacting dimensions. This can inform reflection on previously proposed models. First, it reinforces the inadequacy of a simple contractual or consumer model. While the doctor–patient relationship includes elements of these models (ie the business-transactional dimension), a purely contractual model fails to capture the full nature of the relationship. Several authors have previously highlighted the limitations of the contractual model in response to the increasing corporatisation of medical care.17,28,30,32,33 The current findings add weight to the argument, as reducing healthcare to a primarily commercial enterprise ignores the personal relationship of trust underpinning WPC. A fiduciary model is closer to these findings, as it includes a moral dimension and the doctor’s professional responsibility to act in the patient’s best interests; however, it also implies limitation of patient autonomy.28,29,31 Some authors have described the relationship as a covenant of trust; this perhaps comes closest to capturing the current findings, though does not encompass business-transactional elements.30,32,33 Future research could develop these findings to a robust model of the doctor–patient relationship in current general practice, explore what is considered an ideal model and assess how well these align. The impact of a team approach on doctor–patient relationships and WPC also requires further research.
These findings have several implications. The ‘art’ of the doctor–patient relationship is foundational to WPC and should be valued. This relationship cannot be reduced to a simple consumerist/contractual model and must be considered at both the individual doctor–patient level and in broader health system design to deliver quality WPC. The third article in this series explores factors that affect the provision of WPC and the doctor–patient relationship underlying it at both local and health system levels.
Strengths and limitations of the study methodology are discussed in part one.5 Additionally, the researchers did not aim to explore the nature of the doctor–patient relationship; rather, this emerged as a theme that was foundational to the topic of interest (WPC). The current findings regarding the nature of the doctor–patient relationship, while illuminating, are therefore preliminary and would benefit from further research.
Conclusion
Australian GPs view the doctor–patient relationship as foundational to WPC as it enables personal knowledge of the patient and trust, and facilitates management. Recognising and facilitating this relationship is essential to provide quality WPC.