Primary healthcare, in Australia principally via general practice, is the main determinant of effective and equitable healthcare for the entire population.1 Planning for an adequate general practitioner (GP) workforce remains a challenging balancing act between demand and supply.2 Australian general practice continues to evolve in a changing political and social context, in which GPs are dealing with an ageing population with more chronic conditions and, at the same time, juggling their work and life responsibilities.3 Although many GPs are satisfied with their job,4,5 these demographic and societal changes are affecting their participation in clinical practice. The average number of clinical hours worked by GPs has decreased in recent years,6 with the trend evident across career stages and genders.7,8 Although female GPs work, on average, fewer hours than male GPs,8 male GPs have also been reducing their clinical working hours.9 Many GPs are also diversifying their career structure to include other non-clinical GP-related activities, such as medical education, research and other professional interests.10,11 The shift to flexibility in workload and conditions is evident in Australia and internationally.5,11–13 This flexibility is often associated with the desire to work fewer clinical hours in order to achieve a better work–life balance.5,14
Although evidence from Canada suggests that recent early-career GPs are not working less than later career cohorts,15 many GPs in training do not see themselves working full time in clinical practice.16–19 Yet, little is known about GPs’ clinical practice once they have completed their training and have made the transition to independent practice. An earlier study of early-career GPs looked at up to five years post-Fellowship,20 but there remains a gap in knowledge of the immediate post-Fellowship period. Addressing this gap is important because the early patterns in general practice can establish future intentions,13,19 and thus inform planning for GP workforce capacity and distribution.3
The aim of this study was to establish the prevalence of early-career GPs working full time in clinical practice and the characteristics associated with early-career GPs working full time.
Methods
This cross-sectional questionnaire-based study of former GP trainees who had been registrars in three contiguous regional training organisations (RTOs) in south-east Australia was conducted in 2018. The sample frame for recruitment was the administrative lists of the participating RTOs. These three RTOs train 46% of all Australian general practice registrars.21 Participants were in their first two years of independent practice (being six months to two years post Fellowship) and are referred to hereafter as ‘alumni’. There were 1256 alumni in the sample frame who were eligible and invited to participate in the study. Where consent was given, questionnaire data were linked to data collected during the alumnus’s vocational general practice training. Participants received an email invitation and were given hard copy or electronic options to complete the survey. Two reminder emails were sent out. The full details of the study methodology are described elsewhere.22
Analysis
The primary outcome factor in this analysis was whether an alumnus was working full time or less than full time (LTFT) in clinical general practice. A GP full-time equivalent is defined as 40 hours/week over 46 weeks a year.23 For this study, LTFT was defined as working less than nine sessions per week in clinical general practice, where one session is equal to approximately 3.5 hours (eg a morning session). In a sensitivity analysis, the outcome factor was the number of GP sessions worked per week.
The independent variables encompassed alumni demographics (age; gender; year of Fellowship; relationship status, such as living with a spouse or partner; spouse/partner employment; dependent children; Australian or international medical graduate; the provision of other regular medical work; regional, remote or urban schooling prior to university), current practice characteristics (Australian Government geographic classification using the Modified Monash Model and socioeconomic status of practice location) and vocational training experience (any part-time training as a general practice registrar, rural location during training, low socioeconomic status area during training, failing any examination component).
Descriptive statistics included frequencies for categorical variables and mean values with standard deviations for continuous variables. The frequencies of categorical variables were compared between outcome categories using Chi-squared tests for all variables, except when Fisher’s exact test was used (due to an expected count <5 in 25% or more cells). For continuous variables, mean values were compared using t-tests.
For the primary analysis (outcome full time versus LTFT practice), independent variables were considered for inclusion in a multivariable logistic regression if there was a univariate association with the outcome at P <0.2. Once the model with all significant covariates was fitted, model reduction was assessed. Covariates that were no longer significant (at P < 0.2) in the multivariable model were tested for removal from the model. If removal of the covariate did not substantively change the resulting model, the covariate was removed from the final model. A substantial change to the model was defined as any covariate in the model having a change in the effect size (odds ratio [OR] or coefficient) of greater than 10%.
For the sensitivity analysis using multivariable linear regression (outcome, number of clinical sessions worked), an analogous process of variable selection and model reduction was used.
Statistical analyses were conducted using STATA 14.2 (StataCorp, College Station, TX, USA) and SAS V9.4 (SAS Institute, Cary, NC, USA).
Ethics
The NEXT-UP project received ethics approval from the University of Newcastle Human Research Ethics Committee (Reference number H-2018–0333).
Results
In all, 354 questionnaires were returned from 1256 sent out (response rate 28%).
Of these participating alumni, 337 (95%) reported currently undertaking some work in clinical general practice. The analyses in this study included only those currently working as a GP.
Of the 320 participants working in general practice and with data on the number of sessions worked, 96 (30%; 95% confidence interval [CI]: 25%, 35%) worked full time in general practice and 224 (70%; 95% CI: 65%, 75%) worked LTFT in general practice, with the largest proportion of alumni (26%; 95% CI: 21%, 31%) working eight clinical sessions per week (Figure 1). (Seventeen respondents answered ‘yes’ to the question ‘Do you currently work as a clinical GP?’ but did not continue with the questionnaire and were excluded from the analysis.)
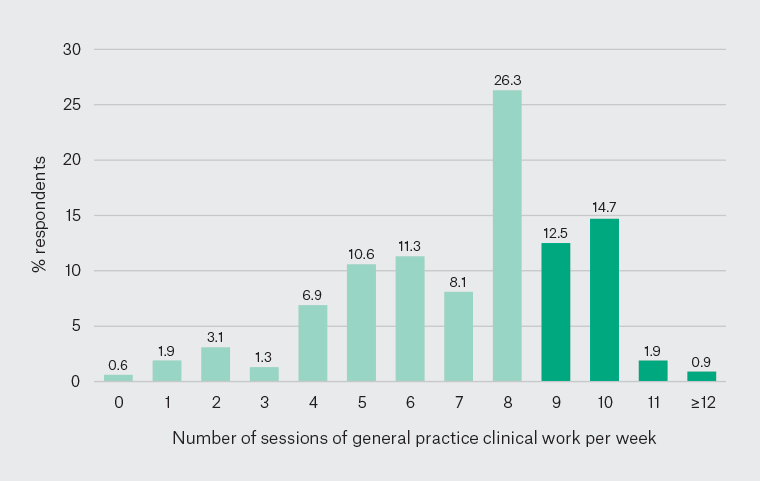
Figure 1. Distribution of alumni’s current number of sessions of general practice clinical work for an average week (light green = less than full time; dark green = full time)
The characteristics of participants and univariate analysis of the alumni’s full-time equivalent status are presented in Appendix 1, and the logistic regression models with dichotomous outcome full time/LTFT are presented in Table 1.
In the adjusted multivariable model, the odds of an alumnus working full time were higher for alumni with a partner than for those with no spouse/partner. Working full time was most strongly associated with having a spouse/partner employed LTFT (OR 4.58; 95% CI: 1.41, 4.9), having a spouse/partner not in the workforce (OR 6.32; 95% CI: 1.7, 23.5) and having failed any examination component (OR 2.45; 95% CI: 1.22, 4.89). The odds of working full time were lower for alumni with dependent children (OR 0.24; 95% CI: 0.11, 0.51), female alumni (OR 0.48; 95% CI: 0.24, 0.96), those whose primary medical degree was obtained in Australia (OR 0.26; 95% CI: 0.12, 0.56), alumni who schooled in a regional or rural area or small town (OR 0.37; 95% CI: 0.16, 0.86), alumni providing other medical work LTFT (OR 0.34; 95% CI: 0.16, 0.71) and alumni who had taken additional leave during training (OR 0.32; 95% CI: 0.14, 0.76).
The findings of the sensitivity analysis (multivariable linear regression; outcome: number of GP sessions worked per week) were similar to those of the primary logistic regression analysis. An additional significant finding of the multivariable analysis was that an older alumnus age was associated with fewer sessions per week being worked (coefficient –0.06; 95% CI: –0.11, –0.02). That is, older early-career GPs are more likely to work LTFT. The characteristics of participants and univariate analysis of alumni’s sessions worked per week are presented in Appendix 2 (summarised as 0–2, 3–5, 6–8 and ≥9 sessions) and the results for the logistic regression models are presented in Table 2.
| Table 1. Early-career general practitioners’ participation in the general practice workforce: Logistic regression models with outcome ‘worked full-time (more than eight sessions per week) in general practice’ |
| |
Univariate |
Adjusted |
| Variable |
Class |
OR (95% CI) |
P value |
OR (95% CI) |
P value |
| Current practice location |
MMM 2–7 |
0.47 (0.27, 0.83) |
0.009 |
0.57 (0.25, 1.30) |
0.18 |
| Relationship status/spouse or partner employment |
Spouse/partner employed full time |
0.62 (0.30, 1.28) |
0.20 |
1.61 (0.65, 3.98) |
0.31 |
| Spouse/partner employed LTFT |
1.21 (0.53, 2.76) |
0.65 |
4.58 (1.41, 14.9) |
0.01 |
| Spouse/partner not in workforce |
1.79 (0.72, 4.47) |
0.21 |
6.32 (1.70, 23.5) |
0.006 |
| Dependent children |
Yes |
0.51 (0.31, 0.83) |
0.007 |
0.24 (0.11, 0.51) |
<0.001 |
| Gender |
Female |
0.38 (0.23, 0.63) |
<0.001 |
0.48 (0.24, 0.96) |
0.04 |
| AMG/IMG |
AMG |
0.42 (0.25, 0.73) |
0.002 |
0.26 (0.12, 0.56) |
0.001 |
| Regional, remote or urban schooling prior to university |
Regional/rural/small town |
0.42 (0.23, 0.77) |
0.005 |
0.37 (0.16, 0.86) |
0.02 |
| Provision of other regular medical work |
Yes |
0.46 (0.26, 0.80) |
0.006 |
0.34 (0.16, 0.71) |
0.004 |
| Any part-time training as a general practice registrar |
Yes |
0.29 (0.15, 0.54) |
<0.001 |
0.49 (0.22, 1.10) |
0.08 |
| Failed any examination component |
Yes |
3.21 (1.80, 5.71) |
<0.001 |
2.45 (1.22, 4.89) |
0.01 |
| Leave during training |
Yes |
0.22 (0.11, 0.45) |
<0.001 |
0.32 (0.14, 0.76) |
0.009 |
| AMG, Australian medical graduate; CI, confidence interval; IMG, international medical graduate; LTFT, less than full time; MMM, Modified Monash Model; OR, odds ratio |
| Table 2. Early career general practitioners’ participation in the general practice workforce: Linear regression models with outcome ‘sessions of GP work undertaken in an average week’ |
| |
Univariate |
Adjusted |
| Variable |
Class |
Coefficient (95% CI) |
P value |
Coefficient (95% CI) |
P value |
| Gender |
Female |
–1.1 (–1.6, –0.51) |
<0.001 |
–0.66 (–1.2, –0.11) |
0.02 |
| Dependent children |
Yes |
–1.3 (–1.8, –0.73) |
<0.001 |
–1.4 (–2.0, –0.80) |
<0.001 |
| Spouse/partner employment |
Spouse/partner employed full time |
–0.68 (–1.5, 0.12) |
0.10 |
0.28 (–0.47, 1.02) |
0.47 |
| Spouse/partner employed LTFT |
–0.34 (–1.3, 0.59) |
0.48 |
0.84 (–0.08, 1.77) |
0.07 |
| Spouse/partner not in workforce |
0.33 (–0.72, 1.38) |
0.54 |
1.33 (0.30, 2.35) |
0.01 |
| AMG/IMG |
IMG |
0.90 (0.28, 1.52) |
0.005 |
1.48 (0.85, 2.10) |
<0.001 |
| Failed any examination component |
Yes |
0.98 (0.33, 1.64) |
0.003 |
0.66 (0.07, 1.26) |
0.03 |
| Other medical work |
Yes |
–1.1 (–1.7, –0.59) |
<0.001 |
–1.1 (–1.6, –0.57) |
<0.001 |
| Any part-time training as a general practice registrar |
Yes |
–1.7 (–2.3, –1.2) |
<0.001 |
–0.67 (–1.2, –0.11) |
0.02 |
| Leave during training |
Yes |
–1.5 (–2.1, –0.93) |
<0.001 |
–0.64 (–1.2, –0.08) |
0.03 |
| Registrar age |
|
–0.03 (–0.07, 0.01) |
0.16 |
–0.06 (–0.11, –0.02) |
0.008 |
| AMG, Australian medical graduate; CI, confidence interval; GP, general practitioner; IMG, international medical graduate; LTFT, less than full time |
Discussion
Main findings and comparison to previous literature
In this study, 95% of early–post Fellowship GPs were working in clinical general practice and, of those, 70% were working LTFT. In a previous study of early-career GPs (up to five years post-Fellowship), 48% reported working fewer than eight sessions per week.20 This compares with 44% in the present study working fewer than eight sessions a week, after adjusting for the 26% of participants who reported working eight sessions per week (Figure 1).
Demographic factors account for most of the statistically significant associations of full-time work. GPs who work full time are more likely to be male, be an international medical graduate, have spouses/partners working LTFT or not in the workforce, not have dependent children, not have been to a regional/rural school prior to university, have failed an examination component during training, not have taken additional leave during training and not do any non-clinical GP work.
The finding in this study that early-career female GPs were more likely to work LTFT than early-career male GPs is consistent with other studies.8 However, most male respondents in this study were also working LTFT, which is in accord with Australian trends.9
Early-career international medical graduates were more likely to work full time than early-career Australian medical graduates. This can be considered in the context of findings that GPs who graduated from an Australian medical school report lower earnings than international medical graduates.24
Interpretation of findings
Relationship and family structure were associated with early-career GPs’ clinical hours. Early-career GPs with a spouse/partner not in the workforce were more likely to work full time than early-career GPs with no spouse/partner. Early-career GPs with dependent children were also more likely to work LTFT than those without dependent children. These associations are not unique to Australia; for example, similar results have been reported from Canada.25
Early-career GPs who provided other medical work were more likely to work LTFT than early-career GPs who did not provide other medical work. In the present study, 38% of early-career GPs working LTFT in clinical general practice were providing other medical work. Some were providing non-GP clinical work (eg surgical assisting, skin cancer clinics, and hospital work, including in emergency departments); others were doing non-clinical work, such as medical administration. The finding that a significant number of early-career GPs are providing other medical work suggests that they may be working full time, combining clinical practice with other professional interests that diversify their skills and knowledge set and improve the work–life balance.10,12,16 Moreover, the contributions that GPs make to other areas of work, such as medical education, are essential in the promotion of general practice to medical students and to the training of general practice registrars.26,27
Two statistically significant findings were related to vocational training experience. Early-career GPs who had failed any examination component were more likely to work full time compared with early-career GPs who had not failed any examination component. Why this is so is not clear; a recent qualitative study from the UK found an interrelated combination of professional, personal and social factors contributed to GP trainees struggling and failing clinical examinations.28 Early-career GPs who had taken extra leave during training were more likely to work LTFT than early-career GPs who had not taken extra leave during training. Some of this difference may be explained by registrars who become parents during training.29 Female GPs are less likely than their male counterparts to work full time, both during training and in independent practice.12
Study strengths and limitations
The overall response rate in this study was 28%. Although this is consistent with surveys of Australian GPs,30 there is potential for non-response bias, and the direction of any potential bias is uncertain. Given this caveat, the participants in this study trained in areas covering major cities and regional, rural and remote areas, and have a similar demographic profile (66% female, mean age 36 years, 30% international medical graduates; refer to Appendix 1) to the Registrar profile in the 2019 National Registrar Survey (63% female, 55% aged 30–39 years, 31% international medical graduates),21 which suggests generalisability to the wider Australian general practice training program. The impact of COVID-19 on the working hours of early-career GPs may affect the results if the study were to be repeated. A limitation of the study, common to all cross-sectional studies, is that causal relationships cannot be inferred from the associations and correlations established in this study. A further limitation may be that there is not a standard definition of ‘full time’. However, the findings of the primary analysis in this study were supported by the sensitivity analysis.
Implications for policy and further research
Planning for an adequate primary care workforce that is responsive to the changing needs of the Australian population will require an understanding of the practice patterns of GPs.6 A focus on early-career GPs can provide relevant information on the working trends of recent fellows. Further cohort studies that follow early-career GPs over time, along with qualitative research components, are warranted to develop a deeper understanding of these trends.
Conclusion
This study confirms that many early-career GPs are choosing to work LTFT in clinical practice. The findings establish that, in the transition to independent practice, factors such as spouse/partner employment and family structure coincide with working LTFT in clinical general practice. Significantly, many early-career GPs working LTFT in clinical general practice provide other medical work that uses their skills and knowledge, which warrants further qualitative investigation.